- What is endometriosis?
- Symptoms of endometriosis
- Do you have endometriosis?
- When to see your doctor
- How endometriosis can affect your life
- Causes of endometriosis
- Risk factors for endometriosis
- Can you prevent endometriosis?
- Endometriosis and other health conditions
- Getting a diagnosis for endometriosis
- Treatments for endometriosis
- Endometriosis at different life stages
- Living with endometriosis
- Watch this video – yoga for endometriosis
-
Reviewed
-
Last updated:November 11 2025
-
Last reviewed:November 11 2025
Key takeaways
- We don’t know the exact cause of endometriosis – it’s a complex condition that depends on the oestrogen hormone.
- Common symptoms of endometriosis include severe period pain, painful sex, infertility, persistent pelvic pain and heavy periods.
- The recommended way to see if you have endometriosis is with imaging technology, such as ultrasound.
- See your doctor if you have severe period pain that stops you from doing everyday activities, such as school and work.
Sections on this page
- What is endometriosis?
- Symptoms of endometriosis
- Do you have endometriosis?
- When to see your doctor
- How endometriosis can affect your life
- Causes of endometriosis
- Risk factors for endometriosis
- Can you prevent endometriosis?
- Endometriosis and other health conditions
- Getting a diagnosis for endometriosis
- Treatments for endometriosis
- Endometriosis at different life stages
- Living with endometriosis
- Watch this video – yoga for endometriosis
Key takeaways
- We don’t know the exact cause of endometriosis – it’s a complex condition that depends on the oestrogen hormone.
- Common symptoms of endometriosis include severe period pain, painful sex, infertility, persistent pelvic pain and heavy periods.
- The recommended way to see if you have endometriosis is with imaging technology, such as ultrasound.
- See your doctor if you have severe period pain that stops you from doing everyday activities, such as school and work.
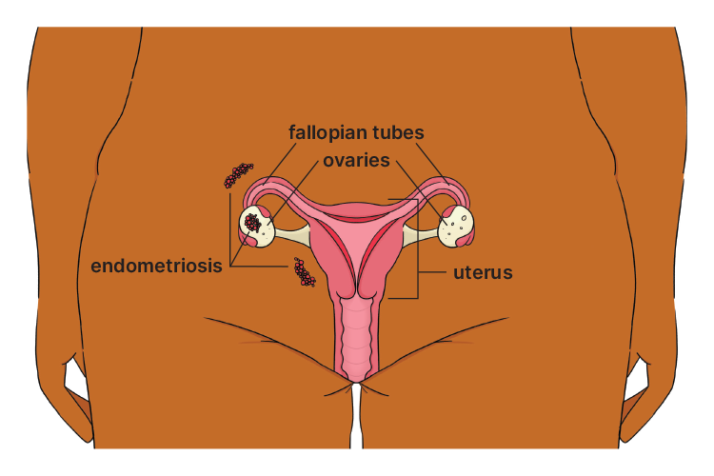
What is endometriosis?
Endometriosis is a condition where tissue, similar to the lining of the uterus, grows in other parts of your body. The tissue that grows outside your uterus bleeds around the time you have your period.
Endometriosis is associated with pain and inflammation.
In Australia, one in 7 women have been diagnosed with endometriosis.
Most endometriosis grows in the pelvic area.
For example:
- the tissue that lines the abdominal wall
- cysts on the ovaries.
More rarely, endometriosis can be found outside the pelvic area.
Symptoms of endometriosis
People with endometriosis can have different symptoms. The severity of symptoms is not related to the number or extent of endometriosis lesions a person has.
Different factors can cause endometriosis symptoms to get better or worse over time. For example, treatments, age and a person’s environment.
- severe period pain
- deep pain during or after sex
- infertility
- persistent pelvic pain
- heavy periods
- bowel symptoms (e.g. bloating, constipation, diarrhoea or pain when doing a poo)
- feeling very tired
- back pain
- sleep problems
- headache
- urinary symptoms (e.g. pain when weeing or blood in your wee)
- allergies
Some women who have endometriosis also have persistent pelvic pain (PPP). PPP is pain in your pelvic area that’s felt most days and lasts for more than 6 months.
If your endometriosis symptoms stop you from doing day-to-day activities, for example, work, study or exercise, see your doctor. It’s also a good idea to see your doctor if your symptoms are getting worse or making you feel anxious or depressed.
Lived experience

-
Story
Do you have endometriosis?
Use this handy checklist to record your symptoms and how they affect you. Take it with you when you visit your doctor.
-
Download the checklistViewpdf • 119 KB
When to see your doctor about endometriosis symptoms
Pain is a common symptom of endometriosis. But it’s not normal to have severe period pain.
If you think you have endometriosis, see your doctor as soon as possible.
Your doctor may ask questions about:
- your periods, for example, if your periods are regular and if you have heavy bleeding
- period pain, for example, where you have pain, how long the pain lasts, if the pain stops you from doing normal activities and what medicines help to reduce the pain
- different types of pain, for example, if you have pain during or after sex or when you go to the toilet
- different types of symptoms, for example, if you have constipation, diarrhoea or bloating; lower back or leg pain; or fatigue
- your family history, for example, if family members have had endometriosis
- your fertility, for example, if you have tried to get pregnant.
How endometriosis can affect your life
Endometriosis can be tough, impacting your physical and mental health.
Causes of endometriosis
It’s not yet known exactly how and why some women develop endometriosis. It’s a complex condition that depends on the oestrogen hormone. But it may also be influenced by other factors.
Backwards (retrograde) menstruation
When you have a period, blood flows out of your vagina. But it can also flow backwards along your fallopian tubes into your pelvic area. Nearly all women experience this, but the blood (which contains endometrial cells) is usually absorbed or broken down in the body. In some women, the endometrial tissue starts to grow and form lesions.
Genetics
Genetics play an important role, but genetics don’t fully explain why some women develop endometriosis and others don’t.
How body systems work
Researchers are looking at different factors that might cause endometriosis. For example, how the immune and hormone systems interact.
Risk factors for endometriosis
We need more research to show how genetics can increase the risk for endometriosis, and to identify the genes involved.
You can’t change some potential risk factors for endometriosis, such as your birth weight and when your first period started. But you can seek help early if you have symptoms such as severe period pain.
Can you prevent endometriosis?
There is no known way to prevent endometriosis. We need more research to understand what actions might help to reduce the risk of developing the condition.
Endometriosis and other health conditions
Some other health conditions are more likely in women with endometriosis, but we need more research to better understand this. It’s helpful to be aware of the links, but it doesn’t mean you will develop these conditions:
- depression and anxiety
- other chronic pain conditions, such as migraine
- uterine fibroids (non-cancerous tumours that grow into the wall of the uterus).
- adenomyosis (where tissue that normally lines the uterus grows into the muscle wall)
- ovarian, breast, endometrial and thyroid cancer (although the risk is small)
- autoimmune diseases, such as lupus, rheumatoid arthritis or inflammatory bowel disease
- early menopause
- cardiovascular disease.
Getting a diagnosis for endometriosis
It can take several years to get a diagnosis for endometriosis. This is because symptoms vary between women, symptoms can change over time and some symptoms overlap with other conditions. Also, period pain is often accepted as normal.
It’s good to know that the time taken to get a diagnosis is decreasing as awareness and medical knowledge get better.
Early diagnosis and treatment of endometriosis will help you manage the condition and improve your quality of life.
The recommended way to see if you have endometriosis is with imaging technology, such as ultrasound.
Pelvic or abdominal examination
When you visit your doctor, they will ask about your symptoms and medical history. They may also suggest an internal examination to feel for things like tenderness, areas of thickening or lesions in the vagina. The examination can also help rule out other causes of symptoms.
If your doctor suspects endometriosis, you may be referred to a specialist for an ultrasound.
Ultrasound
In Australia, an internal ultrasound is the recommended way to look for signs of endometriosis. A device that records images of the pelvic area is inserted into the vagina. This gives a more accurate result than an ultrasound on your belly.
The internal ultrasound scans are good at showing endometriosis, but they aren’t perfect. You may still have the condition, even if the scan doesn’t show signs of endometriosis.
Depending on the results, your doctor might recommend certain medicines to manage symptoms, or they may offer surgery. But the aim is to minimise surgery where possible.
If you can’t have an ultrasound, your doctor may recommend an MRI.
Magnetic resonance imaging (MRI)
MRI is a technology used to take cross-sectional pictures of your body. MRI scans are best reviewed by specialists in this type of imaging. The scans show how much deep endometriosis is in your body and helps inform decisions about surgery.
Laparoscopy
A laparoscopy is keyhole surgery (via the belly) performed under general anaesthetic. A laparoscopy can confirm the presence of endometrial tissue, which can be treated during the operation.
This surgery is usually performed if your doctor thinks you may have endometriosis and other treatments haven’t worked. But surgery comes with risks, so it’s important to minimise this procedure where possible.
If you choose to have surgery, look for a surgeon who has experience managing endometriosis.
Stages of endometriosis
Several staging systems have been created to show different levels and forms of endometriosis. Each system has its strengths and weaknesses.
Knowing about stages can help you understand endometriosis. But it’s important for you and your doctor to focus on your symptoms, preferences and priorities when making treatment decisions.
Revised American Society for Reproductive Medicine (rASRM) stages of endometriosis:
- Stage 1 – minimal (a few superficial implants).
- Stage 2 – mild (more and deeper implants)
- Stage 3 – moderate (many deep implants, small cysts on the ovaries and adhesions).
- Stage 4 – severe (many deep implants, large cysts on the ovaries and many thick adhesions.
Treatments for endometriosis
Women are more likely to have good long-term outcomes when they get an early referral and help from a specialist medical team. For example, doctors, gynaecologists, surgeons with special training and pelvic floor physiotherapists.
There isn’t a single ‘best’ treatment for endometriosis that works for everyone. Your medical team should consider your symptoms, preferences and priorities when recommending treatment options.
Pain control for endometriosis
Your doctor may recommend pain-relief medicines, such as paracetamol and non-steroidal anti-inflammatory drugs, for example, ibuprofen, for temporary relief. But if they don’t help with the pain, you may need other types of pain management.
Hormone medicines for endometriosis
Hormone medicines aim to reduce pain and the severity of endometriosis by slowing the growth of endometriosis. But symptoms can come back if you stop using these medicines.
Depending on your situation, your doctor may recommend the following medicines:
- the Pill
- progestogen (e.g. pills, injections or IUD)
- gonadotrophin-releasing hormone (GnRH) agonists and antagonists
- combined GnRH antagonist, oestrogen and progestogen pill, known as ‘combined relugolix treatment’.
Talk to your doctor about the benefits and risks of each treatment.
Note that hormone medicines will prevent conception, so they are not recommended if you’re planning to get pregnant.
When you take the Pill continuously, by skipping the sugar (hormone-free) pills, it:
- stops your periods
- may reduce your pain
- may slow the progression of endometriosis.
It also provides contraception if needed. But you don’t need to be sexually active to take the Pill.
Possible side effects include:
- nausea
- headache
- weight gain
- bleeding between periods
- mood changes
- blood clots.
Your doctor may not recommend the Pill in some cases. For example:
- if you have a history of blood clots, heart disease or migraine with aura
- are over the age of 35 and smoke
- have breast cancer
- have severe liver disease.
Progestogens (natural and synthetic forms) relieve pain for many women with endometriosis.
You can take progestogens as a daily pill, or you can choose a long-acting option such as an injection or IUD.
Possible side effects include:
- headache
- tender breasts
- irregular bleeding
- absent periods
- acne
- mood changes.
If you have severe symptoms, and you’ve tried other treatments like the Pill or progestogens, your doctor may recommend GnRH treatment. It’s important to ask about the benefits and risks before taking this treatment.
GnRH treatment creates a temporary medically induced menopause, which may cause menopausal symptoms and increase the risk of developing osteoporosis.
This treatment may be recommended for women with moderate to severe pain and women whose symptoms haven’t improved after other medicines or surgery.
Endometriosis medicine is now cheaper
The progestin medicine, dienogest, used to treat endometriosis, has been added to the Australian Pharmaceutical Benefits Scheme (PBS). This means the medicine is a lot cheaper.
Non-hormone medicines for endometriosis
Some antidepressant medicines affect the central nervous system’s response to pain. These medicines may help manage persistent pelvic pain associated with endometriosis.
Surgery for endometriosis
Most surgery for endometriosis is performed via keyhole surgery (laparoscopy). The aim of surgery is to remove endometriosis lesions, repair damage to organs and improve symptoms. It’s important to choose a surgeon with lots of experience in this field.
The first operation has the best chance of removing the endometriosis. Additional surgeries may cause scarring and be less effective. Every surgery comes with the risk of complications, so it’s important to minimise surgeries where possible.
If endometriosis is in the bowel or bladder, the procedure is more complex and other specialists, for example, a urologist or bowel surgeon, may be involved in the surgery.
We need more research to prove that surgery reduces pain or quality of life for people with endometriosis. After surgery, symptoms come back in about 40% of women.
A hysterectomy is an operation to remove the uterus (womb), cervix and fallopian tubes. The ovaries are usually left in the body to minimise the risk of medically induced menopause.
This surgery may be performed if you have severe pain or heavy menstrual bleeding and have tried all other options to improve your symptoms. It should only be performed if you don’t want to get pregnant in the future.
There is limited evidence to show that endometriosis symptoms improve after a hysterectomy. Endometriosis can also return after a hysterectomy.
It’s important to discuss the risks and benefits of this operation with your doctor before making a decision.
Combined treatments for endometriosis
Talk to your doctor about a combination of surgery and ongoing hormone medicines. If you don’t plan to get pregnant straight after surgery, they may recommend you use hormone therapy to reduce pain and the return of symptoms.
Other treatments for endometriosis
Many people use non-medical options to manage symptoms of endometriosis. For example:
- cognitive behavioural therapy (CBT)
- diet
- yoga
- acupuncture.
These options may help you cope with endometriosis symptoms. But more research is needed to show their effectiveness.
Natural therapies for endometriosis
Some women use natural therapies to manage their symptoms and improve their quality of life.
Natural therapies include supplements (vitamins, minerals and fish oils), herbal medicine (tea, tablets and liquids) and nutrition.
There haven’t been many large studies about the effectiveness of natural therapies in managing endometriosis symptoms.
Note that natural therapies should be prescribed by a health practitioner trained in their use. It’s important to tell your doctor if you use these, as some natural therapies can affect other prescribed medicines.
Omega-3 fats are often recommended for endometriosis to help with inflammation and chronic pain. You can increase the amount of omega-3 fats in your diet by eating oily fish, linseeds, flaxseed oil, hemp seeds and walnuts. You can also take supplements. More research is needed to understand how omega-3 fats might help with inflammation.
Herbal medicines used to reduce inflammation and pain include ginger and turmeric. While there is some evidence that these medicines may help inflammation-based conditions, more studies are needed in this area.
Traditional herbal medicines used for general period pain include cramp bark, black haw and wild yam. But there isn’t enough evidence to suggest these medicines are effective for treating endometriosis-related pain.
A few small studies have explored the use of magnesium supplements to reduce general period pain. The results are promising, but larger studies are needed to confirm the findings.
Smaller studies have found that acupuncture may reduce endometriosis-related pain. But larger, higher-quality trials are needed in this area.
Traditional Chinese medicines may also be recommended for conditions such as endometriosis, but more studies are needed to understand how they work and if they are effective.
Endometriosis at different life stages
Endometriosis symptoms can impact many aspects of your life. These may vary depending on your life stage.
Endometriosis in teenage years
It can take time to get a diagnosis of endometriosis in teenage years. But with more awareness of the condition and its symptoms, doctors are identifying endometriosis earlier.
Symptoms such as pain before and during a period, pain between periods and nausea with pain are common in teenage years. But these symptoms may not be due to endometriosis.
If your doctor suspects endometriosis, they may recommend an ultrasound on the abdominal area to learn more.
They may suggest hormone medicines, such as the Pill or progestogen-only therapy, to help with painful periods. If symptoms don’t get better after several months of hormone medicines, doctors may suggest surgery.
Your doctor can refer you to a gynaecologist with specialist skills in treating endometriosis in teenage years.
Endometriosis, fertility and pregnancy
Endometriosis may impact your fertility and plans to become pregnant.
Research suggests women with endometriosis are twice as likely to experience infertility as those without the condition. But not all people with endometriosis have trouble getting pregnant.
If you feel worried or depressed about having endometriosis and fertility problems, talk to your doctor, counsellor or psychologist. They can help you understand the diagnosis and your options, such as fertility treatment.
Lived experience story

-
Story
Endometriosis and menopause
Endometriosis symptoms often improve after menopause due to the drop in oestrogen hormone levels.
But menopause is not a ‘cure’ for endometriosis. Some women continue to have symptoms after natural or medically induced menopause.
If you have endometriosis and are using menopausal hormone therapy (MHT) to manage menopausal symptoms, it’s recommended you use combined MHT rather than oestrogen-only MHT.
Living with endometriosis
Endometriosis can affect your physical health and emotional wellbeing. It may also impact your relationships and sex drive.
It’s important to remember you’re not alone. It can be hard to talk about endometriosis and how it affects you. But when people in your life understand the condition, they are better able to support you through your ups and downs.
Endometriosis and physical health
A healthy lifestyle may not reduce the severity of your endometriosis, but it is important to be as healthy as possible when managing this condition.
Physical activity
Physical activity might help you cope with endometriosis by:
- releasing feel-good chemicals that reduce your awareness of pain signals
- reducing inflammation
- helping to relax your pelvic floor muscles
- improving your range of movement around your hips and pelvic area
- improving your mood
- reducing fatigue.
It may also improve constipation, bloating and bowel pain, and protect against other diseases and health issues, for example, cancer, diabetes and heart disease.
Sometimes physical activity can have side effects, for example, a pain flare, so it’s important to break your exercise into small sessions throughout the day or try different types of activity like walking or yoga.
Aim to do 20 to 30 minutes of exercise most days of the week. If you haven’t done any exercise for a while, ease into your exercise program and gradually build up your fitness levels.
-
Read our factsheet about how to pace your physical activityViewpdf • 225 KB
Watch this video – yoga for endometriosis
In this video, Dr Pav Nanayakkara, gynaecologist and advanced laparoscopic surgeon at Jean Hailes Clinics, guides you through some yoga poses for period pain relief.
Sleep
Quality sleep will help you function at your best. Try to:
- have regular sleep and waking times
- reduce or stop drinking alcohol and coffee
- avoid eating heavy meals late at night.
Diet
While there is no direct evidence that nutrition influences endometriosis, a healthy diet is important for overall wellbeing. This includes lots of plant-based foods, for example, fruit, vegetables, nuts, seeds, legumes, as well as fish.
If you experience bowel symptoms, it’s helpful to learn which foods trigger these symptoms. Try keeping a food diary to track how your diet affects you. If you find you are sensitive to certain food types, ask your doctor to refer you to a dietitian with experience in this area.
Endometriosis and emotional wellbeing
Living with endometriosis can affect your emotional wellbeing, especially if you experience pain. Depending on your diagnosis and situation, you may have different emotions, ranging from shock and anger to sadness and depression.
It can take several years to get a diagnosis of endometriosis. This is a long time to suffer without knowing the cause or getting the right treatment.
Your feelings may vary depending on:
- the severity of your symptoms
- how long you’ve had symptoms
- how long it’s taken to get a diagnosis
- your treatment options
- your stage of life
- your support networks.
Body image
Body image is the way you think and feel about your body.
Some women with endometriosis have a negative body image due to physical symptoms such as pain, fatigue, bloating, painful sex, irregular periods and bladder and bowel problems.
If your body image is negatively affecting your emotional wellbeing, seek help from a counsellor or psychologist with experience in endometriosis and body image.
For more information about body image, visit the Butterfly Foundation website.
Stress
Endometriosis symptoms can be unpredictable and distressing. You might also feel stressed and frustrated before diagnosis, especially if you’ve been misdiagnosed or your symptoms have been dismissed. It’s important to find a doctor who listens and investigates your concerns.
Too much stress, particularly over a long period of time, can take its toll on your health and wellbeing. For example, ongoing stress can cause physical reactions such as nausea, diarrhoea, overeating or undereating.
It’s important to understand what is causing you stress and find ways to manage it. For example:
- try gentle yoga or mindfulness therapy
- find time in your day to do things you love
- seek help from a psychologist or counsellor if needed.
Anxiety
If you have endometriosis, you may experience anxiety. Anxiety involves extreme feelings of fear and worry. Physical symptoms might include a racing heart, rapid breathing and sweating. Psychological symptoms can include worry, over-thinking things and avoiding situations. Anxiety can lead to a loss of confidence and avoidance of people and places.
Depression
Some women with endometriosis get depression. Depression is more than feeling sad. It involves constant and intense negative thoughts and feelings. If you have depression, you might:
- feel tired all the time
- lose confidence
- lose interest in things you used to love doing
- find it hard to concentrate
- have different eating and sleeping patterns.
When to get help
It’s important to ask for help if endometriosis affects your mental and emotional wellbeing. Your doctor can write a referral for you to see a psychologist or counsellor. You can get a Medicare rebate for a set number of sessions with psychologists and allied health professionals.
It might help to join a local support group so you can talk to other women going through a similar experience.
Visit the Endometriosis Australia website to find a support group near you.
Endometriosis, relationships and sex
Chronic pain can impact different relationships in your life.
Lifestyle factors can affect how you experience pain. For example, stress and poor sleep can make the pain feel worse.
It’s common for women with chronic pain to have a lowered sex drive (libido). Sex drive varies for each person, and it can be influenced by different factors. For example, your health, stress levels, mood and relationships.
Many women with endometriosis experience painful sex. This pain is often deep in the vagina, but it can also be near the vaginal entrance and in the lower tummy. Pain with sex can come from endometriosis implants, an overactive pain system and overactive muscles, including pelvic floor muscles.
When you experience pain, it can be hard to relax your pelvic floor muscles. This can cause more pain, which may reduce your sex drive.
How to improve your sexual experience
If you experience painful sex, don’t just put up with it. The good news is, there are many practical things you can do to improve your sexual experience.
A qualified pelvic floor physiotherapist can teach you how to relax your pelvic floor muscles. They can also help with different methods to relieve pain and manage persistent pain.
If you’re in a relationship, it’s important for you and your partner to discuss your feelings and seek help from a psychologist or relationship counsellor if needed. And remember, you can enjoy intimacy in many ways other than sexual intercourse.
Our review process
This information has been reviewed by clinical experts and is based on the latest evidence.
Our content review process ensures our health information is accurate, trustworthy, current and useful.
We regularly check our information to make sure it reflects the latest clinical guidelines and key findings from large, reliable studies.
Where possible, we focus on Australian research to make our information more relevant locally.
Experts play a key role in reviewing our content. Clinicians at Jean Hailes check information for accuracy and real‑world relevance. These include GPs, gynaecologists, endocrinologists, psychologists and allied health professionals.
We also work with partner organisations, independent specialists and people with lived experience to make sure our content reflects both expert knowledge and the experiences of the community.