- What is menopause?
- What is perimenopause?
- What is postmenopause?
- How do you know if you’ve reached menopause?
- How do you know if you are in perimenopause?
- Perimenopause and menopause checklist
- Menopausal symptoms
- Other health issues and concerns
- Hormones and menopause
- Fertility and contraception around menopause
- Health after menopause
- When to see your doctor
- Premature and early menopause
- Medically induced menopause
- Menopausal symptom treatments
- Managing menopausal symptoms
- Looking after yourself around the time of menopause
- Menopause for partners
-
Reviewed by:
Key takeaways
- Menopause is when you have your final menstrual period. It typically occurs between the ages 45 and 55 in Australia.
- Perimenopause is the time leading up to and just after menopause. If you have menopausal symptoms, they will likely start in perimenopause.
- Postmenopause is the rest of your life after menopause. Some people will have menopausal symptoms that continue into postmenopause.
- A lot of people use the word ‘menopause’ to describe the whole transition from perimenopause to postmenopause.
- Common menopausal symptoms include hot flushes, night sweats, and vulval and vaginal problems. Menopause might also affect other things like sleep, mental health, sex drive, memory and concentration
- Everyone has a different experience of menopause. Some people have no or mild symptoms and some have severe symptoms.
- Menopausal hormone therapy (MHT; also called hormone replacement therapy or HRT) is the most effective medicine for managing symptoms but might not be right for everyone.
- If menopausal symptoms are affecting your daily life, see a doctor for support. No-one should put up with symptoms that affect their ability to do their daily activities or their quality of life.
Sections on this page
- What is menopause?
- What is perimenopause?
- What is postmenopause?
- How do you know if you’ve reached menopause?
- How do you know if you are in perimenopause?
- Perimenopause and menopause checklist
- Menopausal symptoms
- Other health issues and concerns
- Hormones and menopause
- Fertility and contraception around menopause
- Health after menopause
- When to see your doctor
- Premature and early menopause
- Medically induced menopause
- Menopausal symptom treatments
- Managing menopausal symptoms
- Looking after yourself around the time of menopause
- Menopause for partners
Key takeaways
- Menopause is when you have your final menstrual period. It typically occurs between the ages 45 and 55 in Australia.
- Perimenopause is the time leading up to and just after menopause. If you have menopausal symptoms, they will likely start in perimenopause.
- Postmenopause is the rest of your life after menopause. Some people will have menopausal symptoms that continue into postmenopause.
- A lot of people use the word ‘menopause’ to describe the whole transition from perimenopause to postmenopause.
- Common menopausal symptoms include hot flushes, night sweats, and vulval and vaginal problems. Menopause might also affect other things like sleep, mental health, sex drive, memory and concentration
- Everyone has a different experience of menopause. Some people have no or mild symptoms and some have severe symptoms.
- Menopausal hormone therapy (MHT; also called hormone replacement therapy or HRT) is the most effective medicine for managing symptoms but might not be right for everyone.
- If menopausal symptoms are affecting your daily life, see a doctor for support. No-one should put up with symptoms that affect their ability to do their daily activities or their quality of life.
What is menopause?
Menopause is when you have your final menstrual period. Your periods stop because your ovaries stop producing certain hormones and stop producing eggs.
Read more about hormones and menopause.
In Australia, most women (around 3 in 4) reach natural menopause between the ages of 45 and 55 years, but it can happen earlier or later. The average age of natural menopause is 51.
Some women (around 1 in 5) experience premature or early menopause, which is when menopause occurs before the age of 45 years.
- Premature menopause occurs when menopause happens before the age of 40 years.
- Early menopause occurs when menopause happens between 41 and 45 years of age.
Some women experience medically induced menopause, which is when menopause is caused by medical treatment, such as surgery, chemotherapy, radiotherapy or some medicines.
Some people use the words ‘menopause’ or ‘the menopause transition’ to describe the whole transition from perimenopause (before the final menstrual period) to postmenopause (after the final menstrual period).
Watch this video to get an overview of menopause
Speaker: All women will go through menopause. It’s when periods stop, and it usually happens between the ages of 45 to 55 years.
Although about one in 10 women can go through menopause at younger ages, many women notice changes in the pattern of their periods for a year or two before they completely stop.
Women may notice changes in their bodies around the time of menopause, and each woman’s experience will be different due to traditions, culture, health, and the passage of time.
Some body changes include muscle and joint pains, suddenly feeling hot and sweating, dryness in the vagina, which can cause sex to be painful, trouble going to sleep, or staying asleep and changes in mood. These are usually temporary symptoms and many women can manage these without treatment.
Not everything about menopause is bad. A good thing is not having periods anymore or worrying about getting pregnant unintentionally. Some women as they get older, become more self-confident and find they have more time for themselves.
There are things you can do to feel better during menopause. You can eat healthy food, get more exercise, learn relaxation practises. Join a community group or visit friends, take classes, get a job, or enjoy time at work.
Many women don’t need medical help to manage menopause, but if you are bothered by symptoms or body changes or worried about your health, talk to your doctor.
To find out more about menopause or women’s health in general, visit jeanhales.org.au
End of transcript
What is perimenopause?
Perimenopause refers to the time from when your menstrual periods start changing, or you start having menopausal symptoms, to one year after your final menstrual period (menopause).
Some people use the word ‘menopause’ to cover the whole transition from perimenopause to postmenopause.
During perimenopause, the hormones produced in your ovaries change. This causes your menstrual periods to change and, for some women, menopausal symptoms to start.
In Australia, perimenopause usually starts at around the age of 47. On average, it lasts 4 to 6 years, but for some women it could be shorter or longer.
During perimenopause, you might still ovulate (produce an egg) some months. This is why it is important to consider fertility and contraception during perimenopause.
When to see your doctor
Talk to your doctor if you:
- feel very tired or fatigued (to rule out loss of iron from heavy periods)
- have symptoms that are interfering with your daily activities, including exercise and work, your relationships or your quality of life
- have increased premenstrual syndrome (PMS) symptoms during perimenopause
- you have concerns about your emotional or mental health.
What is postmenopause?
Postmenopause starts one year after your final menstrual period (when perimenopause ends). You are in postmenopause (or, you are ‘postmenopausal’) for the rest of your life.
As your body adjusts to lower hormone levels you might have fewer or less troubling menopausal symptoms. For some women, though, menopausal symptoms extend into postmenopause.
It’s important to look after your health after menopause. Menopause, ageing or a combination of both increases your risk of developing certain health conditions.
When to see your doctor
Talk to your doctor if:
- a menstrual period or bleeding from the vagina after menopause (more than 12 months after your last menstrual period)
- symptoms that are interfering with your daily activities, including exercise and work, your relationships or your quality of life
- you have concerns about your emotional or mental health.
How do you know if you’ve reached menopause?
You have reached menopause if you haven’t had a menstrual period for 12 months.
It’s a good idea to start tracking your menstrual periods when they start changing, so you know when 12 months have passed since you last had a menstrual period.
After you reach menopause, you are in postmenopause (or you are ‘postmenopausal’) for the rest of your life.
It is more difficult to know if you have reached menopause if you do not have menstrual periods. For example, you might not have menstrual periods because you use an IUD (intrauterine device) for contraception or you have had a hysterectomy (an operation to remove your uterus). You can:
- keep a detailed journal (a record) of any menopausal symptoms (when they occurred, how they affected you) for at least 3 months
- take that journal to your doctor, who can use this information to consider further tests.
Remember that something affecting your health at midlife (45-55 years) might not be due to menopause. Midlife is the perfect time to get a thorough check-up from your doctor to check your general health, even if you are not experiencing any symptoms.
Use the Perimenopause and menopause symptom checklist as a tool to help identify your symptoms.
When to see your doctor
Talk to your doctor if:
- You are younger than 45 and your periods are irregular or have stopped
- You have symptoms that are interfering with your daily activities, including exercise and work
- You have symptoms that are affecting your mental health or your relationships
- You have not had a menstrual period for 12 months, and you then have a period or bleeding from the vagina.
Tests to diagnose menopause
It is not usual for doctors to measure hormone levels for a diagnosis if you are in the expected age range for menopause (45 to 55 years). Your doctor will assess your symptoms and whether and how your periods have changed.
Your doctor might do blood tests to check your general health or to rule out any other causes of symptoms.
If you are younger than 45 years and your periods are irregular or have stopped, your doctor will probably measure your hormone levels to understand what’s causing the change.
Some companies sell blood or saliva tests to do at home to diagnose menopause or predict when menopause will happen. These tests are not recommended.
Watch videos about menopause in your language
Find out what happens to your body during menopause and how to manage menopausal symptoms. You can watch the video in Mandarin or Vietnamese.
How do you know if you are in perimenopause?
The most reliable sign you are in perimenopause (or you are ‘perimenopausal’) is if your menstrual periods have become:
- Irregular
- Shorter or longer than usual
- Lighter or heavier than usual
- Absent for a few months.
Some women might start to experience menopausal symptoms in perimenopause, with hot flushes and night sweats the most common.
It is more difficult to know if you have reached menopause if you do not have menstrual periods. For example, you might not have menstrual periods because you use an IUD (intrauterine device) for contraception or you have had a hysterectomy (an operation to remove your uterus). You can:
- keep a detailed journal (a record) of any menopausal symptoms (when they occurred, how they affected you) for at least 3 months
- take that journal to your doctor, who can use this information to consider further tests
Remember that some health issues and concerns at midlife (45 to 55 years) might not be due to menopause. Midlife is the perfect time to get a thorough check-up from your doctor to protect your future health and wellbeing, even if you are not experiencing any challenging symptoms.
Use the Perimenopause and menopause symptom checklist as a tool to help identify your symptoms and talk to your doctor if something doesn’t feel right.
When to see your doctor
Talk to your doctor if:
- You are younger than 45 and your periods are irregular or have stopped
- You have symptoms that are interfering with your daily activities, including exercise and work
- You have symptoms that are affecting your mental health or your relationships.
Tests to diagnose perimenopause
It is not usual for doctors to measure hormone levels to check if you are in perimenopause if you are in the expected age range for menopause (45 to 55 years). Your doctor will assess your symptoms and whether and how your periods have changed.
Your doctor might do blood tests to check your general health or to rule out any other causes of symptoms.
If you are younger than 45 years and your periods are irregular or have stopped, your doctor will probably measure your hormone levels to understand what’s causing the change.
Some companies sell blood or saliva tests to do at home to diagnose perimenopause or predict when menopause will happen. These tests are not recommended.
Perimenopause and menopause checklist
Use this handy checklist to track your menopausal symptoms. Tick the boxes to show which symptoms are bothering you. Take the checklist with you to your next medical appointment.
Menopausal symptoms
Menopause can affect a woman’s physical (body), mental (psychological) and emotional health. Every woman will experience menopause differently.
Around 1 in 4 women will have no menopausal symptoms. Around 1 in 4 women will have severe menopausal symptoms, which interrupt daily activities and quality of life. The rest (2 in 4 women) will have menopausal symptoms that range from mild and annoying through to symptoms that are difficult to manage.
Menopausal symptoms can be influenced by many things, including:
- Your general health and wellbeing
- Your diet and physical activity
- Whether you smoke or not
- Other stresses in your life, such as work, financial and relationship pressures
- Your own thoughts and feelings about menopause
- How your partner, family, friends or community think and feel about menopause.
If you have menopausal symptoms, they will usually start during perimenopause. For some women, symptoms might continue into postmenopause.
Not all of the health issues and concerns experienced by women in midlife (45 to 55 years of age) are due directly to menopause. Some might be due to ageing, or to other health conditions or to life pressures that affect our wellbeing.
Treatments that help your menopausal symptoms might not help with all the health issues you experience around the time of menopause. To understand and manage your own menopause, you might need to be ready to try different things to improve your health and wellbeing.
All midlife health issues and concerns are important, whether they are caused by menopause or not. Speak with your doctor about any health issue or concern that is affecting your quality of life.
Learn more about managing common symptoms
The most common health issues that improve with treatments for menopausal symptoms are covered below. Information on other common health issues – which might or might not be due directly to hormones – are covered in ‘Other health issues and concerns’.
Changing hormones affect your menstrual cycle. Your menstrual periods might become:
- Irregular (for example, no longer starting when they used to each month)
- shorter or longer than usual
- lighter or heavier than usual
- absent for a few months.
During perimenopause, you might experience extreme tiredness or fatigue due to the loss of iron if you have heavy periods.
Around 3 in 4 women experience hot flushes and night sweats around the time of menopause.
A hot flush begins as a sudden feeling or wave of heat in the face, neck and upper chest. They can also spread over the whole body. Hot flushes often come on suddenly and randomly, and usually last 1 to 5 minutes.
The flushes can feel like a burning, overheating sensation. You might also have reddening of the skin and you might start sweating.
Everyone experiences hot flushes differently. For example, some women have mild, quick hot flushes every now and then. Others have more than 20 a day.
When a flush happens at night, it’s called a night sweat.
Stress and anxiety can influence the number and severity of hot flushes. Certain (spicy) foods, alcohol, smoking and being overweight have also been linked to more and more severe hot flushes and night sweats.
It’s common for your sleep patterns to change during perimenopause.
Around 1 in 2 women will have sleep problems during perimenopause and after menopause (in postmenopause). These sleep problems include trouble getting to sleep or staying asleep, and waking too early.
Women who have experienced medically induced menopause are more likely to report severe symptoms of sleep disruption.
Sleep problems can be caused by hormonal changes during menopause. They can also be caused by other factors such as:
- abnormal circadian rhythms (24-hour cycles that regulate sleep and wakefulness)
- having other chronic conditions (e.g. sleep apnoea)
- having other sleep problems (e.g. restless leg syndrome)
- life stresses, such as caring concerns or financial pressures
- poor mental health (e.g., depression or anxiety)
- general ageing.
It is important to address poor sleep, as this has been linked to developing cardiovascular disease, obesity, mood disorders, diabetes and cancer.
Visit the Sleep Health Foundation website for more information about menopause and sleep.
Menopause can affect your:
- mental health, which is your psychological wellbeing and how you think, make decisions and cope with daily life
- emotional health, which is how you experience, handle and express your moods, feelings and emotions.
Jean Hailes’ National Women’s Health Survey found that more than 1 in 2 Australian women who had experienced menopausal symptoms in the last 5 years said their mental and emotional wellbeing had been affected by these symptoms.
For most women, mental and emotional wellbeing improves as you get closer to your final menstrual period and in postmenopause.
Remember that menopause might be responsible for some, all or none of the changes in your mental and emotional health. Women in midlife can also have many caring, financial and work pressures. Understanding what is causing mental and emotional health changes is the first step in improving your health and wellbeing.
Mood changes
Many women say that their moods (their temporary state of mind or how they feel) change around the time of menopause. Some women report experiencing more intense or rapidly changing feelings or of feeling more frequently irritable, angry or sad.
Anxiety and depression
During perimenopause, some women will experience a mental health condition, such as anxiety or depression.
If you have a history of anxiety, depression or premenstrual syndrome (PMS) you should watch carefully for signs that your mental health is being affected.
Mental health symptoms to look out for:
- Feeling sad, low or depressed
- Low energy and motivation
- Feeling worried or anxious
- Panic attacks
- Reduced self-esteem or self-worth
- Loss of sex drive (libido).
Visit the Beyond Blue website to learn more about signs and symptoms of depression or anxiety.
Brain fog
Many women report they experience something they describe as ‘brain fog’ during perimenopause, which includes:
- difficulty concentrating or focusing
- confusion
- poor memory
- forgetfulness
- not having the right words
- losing your ‘train of thought’
- slow thought processes.
Around the time of menopause, some women experience aches and pains in their muscles and joints. These aches and pains commonly affect:
- hands
- knees
- hips
- shoulders
- lower back.
These aches and pains might be stronger in the morning and fade later in the day. Some women also report increased pain sensitivity and intensity. Other factors, such as ageing, physical inactivity, past injury or conditions like arthritis can also cause or affect muscle and joint aches and pains.
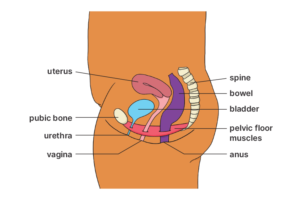
Around 1 in 2 women are affected by ‘genitourinary syndrome of menopause’ (GSM). GSM affects the bladder, vagina and vulva.
Sometimes people will use the term ‘vulvovaginal atrophy’ to describe the changes in the vagina and vulva.
While symptoms such as hot flushes usually disappear over time, bladder, vaginal and vulval problems can continue in postmenopause (and might even get worse).
There are many treatments available, so ask your doctor for recommendations.
Read the Continence Foundation of Australia Guide to bladder and bowel health.
Bladder (urinary) problems
Ageing and menopause can cause your pelvic floor muscles to become weaker. Your pelvic floor muscles help you to hold your wee in.
Menopause also causes your bladder to become less elastic, which means it can’t hold as much wee as it used to. These changes can lead to urinary symptoms such as:
- needing to wee often and with a sense of urgency
- a burning sensation or pain when weeing
- blood in your wee
- wee leakage, especially when coughing, sneezing or laughing
- recurrent urinary tract infections (UTIs).
Vaginal (dry vagina and painful sex) problems
Around the time of menopause, you might experience vaginal dryness and the vagina becomes less elastic. This can lead to painful sex and a loss of sex drive (libido).
Learn more about painful sex and treatment options.
Vulval (irritation) problems
You might experience vulval irritation around the time of menopause. Common symptoms include:
- burning
- itching
- redness
- swelling
- vaginal discharge
- painful sex.
Watch this video about common menopausal symptoms
Professor Rodney Baber, Professor of Obstetrics and Gynaecology, University of Sydney, describes the most common symptoms that women in Australia experience around the time of menopause.
Dr Sarah White (CEO, Jean Hailes for Women’s Health): Jodie in South Australia wants to know: What are the most common symptoms that women in Australia report experiencing during the menopause transition? So, from perimenopause right through to post menopause.
Prof Rodney Baber (Professor of Obstetrics and Gynaecology, University of Sydney): The symptoms that we talk about are the so-called ‘vasomotor symptoms’, which means symptoms that can affect blood vessels and blood flow, and therefore induce changes in our body. Now the commonest of those is the hot flush, or ‘hot flash’ if you come from the United States.
The twin sister of the hot flush is the night sweat, and both of those are heat-losing mechanisms. So your body’s central core body temperature goes up, and it does something to get rid of the heat, and that’s the flush or the sweat. On top of that, the other major symptoms are poor sleep, muscle and joint aches and pains, and mood changes.
So, they’re the critical ones, and often when people refer to vasomotor symptoms, they’re the most common symptoms. And for example, in clinical trials, we know that the most common by far are hot flushes and night sweats, in Western societies, and in Eastern societies, perhaps the most common is muscle and joint aches and pains, followed immediately by hot flushes and night sweats.
End of transcript
Other health issues and concerns
Lack of research on menopause means we have gaps in our knowledge when it comes to all menopausal symptoms and how to treat them.
Some health issues and concerns can be experienced by women around menopause but might not be due directly to hormone changes.
Treatments for menopausal symptoms might help some women with these health issues.
Remember that all midlife health issues and concerns are important, whether they are caused by menopause or not. Speak with your doctor about any health issue or concern that is affecting your quality of life.
Some women experience the thinning and loss of hair around the time of menopause. Not enough research has been done to understand whether hair thinning and loss is caused by the changes and loss of hormones at menopause.
Some women experience a loss of sex drive (also called libido) around the time of menopause. This might be caused by other menopause symptoms, for example, dry vagina, painful sex or poor sleep. Loss of libido might also be due to other reasons.
Some women experience formication, which is described as a sensation of “insects crawling under the skin”, around the time of menopause.
Some women experience skin changes around menopause, including issues like dry skin, itchiness, acne and the appearance of wrinkles.
Women often put on weight around menopause. Menopause itself doesn’t make you put on weight, but some menopausal symptoms (for example, poor sleep) make weight gain more likely. Menopause does change where your weight sits on your body, so you might notice extra body fat around your belly.
Extra belly fat can increase your risk for health conditions such as:
- type 2 diabetes
- heart disease
- dementia
- certain cancers.
Staying active and eating well are important for healthy ageing after menopause.
Hormones and menopause
Hormones are chemicals, made in your body, that relay messages inside your body. They control essential functions, like regulating sleep or hunger.
The main hormones that change as you approach menopause are oestrogen and progesterone. During perimenopause, the amounts of oestrogen and progesterone made by the ovaries swing up and down, causing menopausal symptoms. After menopause, very little oestrogen or progesterone is produced by the ovaries.
Another hormone produced in the ovaries is testosterone. Testosterone does not change because of menopause but starts decreasing in women in their 20s.
Oestrogen
Oestrogen is produced in your ovaries. It is one of the main female sex hormones and plays an important role in the female body.
Oestrogen is needed for:
- the menstrual cycle
- fertility
- pregnancy
- bone strength.
It also helps with brain function and bladder control, and protects you from heart disease.
During perimenopause, the amount of oestrogen produced by your ovaries swings up and down, causing menopausal symptoms. After menopause, the amount of oestrogen produced by the ovaries drops almost to nothing.
Progesterone
Progesterone is also produced in your ovaries. This female sex hormone plays a role in:
- protecting against vaginal problems, like vaginal dryness
- keeping your moods calm
- promoting sleep.
During perimenopause, the amount of progesterone produced by your ovaries swings up and down. After menopause, the amount of progesterone produced by the ovaries drops almost to nothing.
Testosterone
Testosterone is produced by your ovaries but does not change in menopause. This hormone decreases gradually with age starting in your 40s, and increases again at about 58-59 years of age.
Testosterone is not one of the main female hormones but it does have a role in women’s:
- sex drive (libido)
- emotional wellbeing
- bone and muscle strength.
Your doctor might suggest testosterone to help with loss of sex drive.
Fertility and contraception around menopause
You can become pregnant during perimenopause because you might continue to ovulate (produce eggs), even if your periods are irregular.
Fertility naturally declines with age. For women aged 45 to 49 years, the chance of pregnancy is about 2% to 3% per year. After the age of 50, it’s less than 1%.
If you don’t want to become pregnant around the time of menopause, you still need to use contraception.
How long should you use contraception?
If you’re under 50, use contraception until you’ve had 2 years without a period.
If you’re over 50, continue to use contraception until you’ve had one year without a period.
It’s important to know that menopausal hormone therapy (MHT) is not a contraceptive.
There are many types of contraceptive options available. Ask your doctor for more information.
Health after menopause
Postmenopause is the time after your final menstrual period and lasts the rest of your life. The loss of hormones and ageing (or a combination of both) in postmenopause can increase your risk of developing certain health conditions.
Before menopause, women have a lower risk of heart disease than men. After menopause, and as women age, their risk of heart disease increases.
Heart disease is one of the leading causes of death for women in Australia.
After menopause, you may be more likely to develop risk factors for heart disease, including:
- high blood pressure
- an increase in total cholesterol
- an increase in LDL (bad cholesterol)
- a decrease in HDL (good cholesterol)
- an increase in blood fats, such as triglycerides
- weight gain and body fat around the belly.
Women who experience moderate to severe hot flushes and night sweats may have an increased risk of heart disease.
You can reduce your risk of heart disease by focusing on a healthy lifestyle.
You should also see your doctor for a heart check. The doctor will take your blood pressure and organise a blood test. If you have a high risk for heart disease, your doctor may prescribe medicine for high blood pressure and cholesterol.
Articles about heart health
If you want to know more about heart health and heart disease, these articles may be helpful:
The loss of hormones during menopause can lead to loss of bone density. This increases women’s risk of osteoporosis and fractures.
Osteoporosis is a condition where bones become brittle and fragile.
The most rapid bone loss happens in the period around menopause and early postmenopause, mainly in the lower spine. After menopause, the rate of bone loss slows.
It’s important to have regular bone health checks. Your doctor might:
- ask about your medical history
- check risk factors for osteoporosis
- do a bone density test.
Note that Medicare rebates for bone density tests are only available for:
- women with certain risk factors
- women over 70 years of age.
Ageing plus the loss of hormones during menopause can lead to a loss of muscle mass. After menopause, women are at greater risk of developing sarcopenia – a condition where a person loses muscle mass, strength and function, which makes it hard to do everyday activities.
Physical activity is the best way to prevent and manage sarcopenia.
Ageing plus the loss of hormones during menopause can affect your bladder health. These may cause:
- weak pelvic floor muscles
- loss of elasticity of the bladder and pelvic tissues
- thinning of the urethral and bladder lining, which could lead to urinary tract infections (UTIs).
These factors can lead to urinary incontinence (wee leakage). You don’t have to put up with incontinence. Ask your doctor for a referral to a continence nurse or a pelvic floor physiotherapist to help strengthen your pelvic floor muscles.
Sometimes vaginal and vulval symptoms continue after menopause. For example:
- vaginal dryness
- thinning of the vaginal walls
- painful sex.
If these symptoms bother you, ask your doctor about treatment options.
After menopause, you still need regular cervical screening tests until you’re 75 years of age. You’ll need to get tested every 5 years if your results are normal. If your results are abnormal, you will need to do tests more often.
Bleeding from your vagina after menopause is not normal. If you have any bleeding, spotting or staining after menopause, talk to your doctor.
The risk of breast cancer increases as you get older. About 79% of all new cases of breast cancer happen in women over the age of 50.
It’s important to know the normal look and feel of your breasts and talk to your doctor if you notice any changes.
Learn how to stay healthy after menopause in other languages
Watch this short video in Mandarin or Vietnamese.
When to see your doctor
Perimenopause
Talk to your doctor if:
- you feel very tired or fatigued
- you have symptoms that are interfering with your daily activities, including exercise and work, your relationships or your quality of life
- your premenstrual syndrome (PMS) gets worse
- you have concerns about your emotional or mental health.
Postmenopause
Talk to your doctor if you have:
- a period or bleeding from the vagina after menopause
- symptoms that are interfering with your daily activities, including exercise and work, your relationships or your quality of life
- concerns about your emotional or mental health.
Premature and early menopause
Learn about the premature and early menopause, including the causes and how to manage symptoms.
Medically induced menopause
Learn more about medically induced menopause, including what you can do to ease symptoms and reduce health risks.
Menopausal symptom treatments
Learn more about treatments for specific menopausal symptoms.
Managing menopausal symptoms
Learn more about different ways to manage your symptoms, from medical treatments to lifestyle changes.
Looking after yourself around the time of menopause
Learn how to look after your physical and mental health around the time of menopause.
Menopause for partners
Learn how to support your partner during perimenopause and menopause.
Personal stories about menopause

-
Story

-
Story
This content has been reviewed by a group of medical subject matter experts, in accordance with Jean Hailes policy.
© Jean Hailes Foundation. All rights reserved.