-
Reviewed
Key takeaways
- You may need a hysterectomy (removal of your uterus) for different reasons, for example, if you have fibroids, endometriosis or cancer.
- There are 2 types of hysterectomy: total and subtotal
- Ask your doctor about the benefits and risks associated with a hysterectomy before making a decision.
Sections on this page
Key takeaways
- You may need a hysterectomy (removal of your uterus) for different reasons, for example, if you have fibroids, endometriosis or cancer.
- There are 2 types of hysterectomy: total and subtotal
- Ask your doctor about the benefits and risks associated with a hysterectomy before making a decision.
What is a hysterectomy?
A hysterectomy is an operation to remove your uterus. There are many reasons for having a hysterectomy. For example, if you have a health condition, such as:
What are the different types of hysterectomy?
There are 2 types of hysterectomy:
- total hysterectomy
- subtotal hysterectomy.
With both types of hysterectomy, your doctor will usually recommend your ovaries are left behind. This is to reduce the risk of having an earlier menopause.
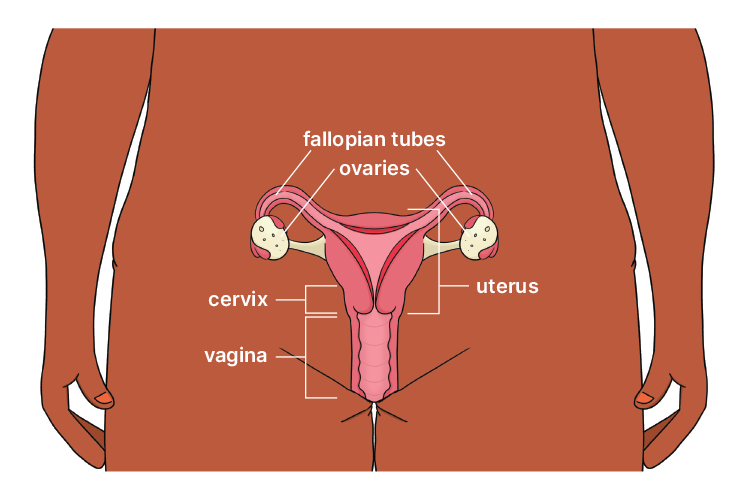
A total hysterectomy involves the removal of your uterus and cervix. Often your fallopian tubes are removed at the same time, as this reduces the chance of ovarian cancer by 60%.
A subtotal hysterectomy involves the removal of your uterus, leaving the cervix in place. Often your fallopian tubes are removed at the same time.
Reasons for having a hysterectomy
Your doctor might recommend you have a hysterectomy for different reasons, including:
- conditions that cause heavy bleeding (e.g. fibroids)
- conditions that cause severe pain and discomfort (e.g. adenomyosis, endometriosis)
- a prolapse (weakness of the tissues supporting your uterus and vaginal walls)
- persistent pelvic pain due to infection or certain health conditions
- chronic pelvic inflammatory disease, sometimes caused by infection in your fallopian tubes and pelvis
- cancer or precancer of your cervix, uterus, ovaries or fallopian tubes.
It can be a big decision to have a hysterectomy as it’s an irreversible procedure. There are many things to consider, such as:
- how your symptoms impact your quality of life
- your plans for future pregnancies.
Do you need a doctor’s referral for a hysterectomy?
Yes, you will need a doctor’s referral to see a specialist (gynaecologist) who can perform the hysterectomy.
How is a hysterectomy performed?
A hysterectomy can be performed in different ways. This will depend on:
- the reason for the procedure
- your medical history
- your overall health.
Hysterectomies are usually performed under general anaesthetic.
Your specialist may perform:
- keyhole surgery (laparoscopy), performed through small cuts in your belly (abdomen)
- surgery via your vagina
- surgery through a cut in your lower belly.
Ask your doctor about the different options and the benefits and risks of each. If you’re still unsure, you can get a second opinion.
What are the risks of having a hysterectomy?
As with any operation, there are some risks associated with having a hysterectomy. For example, you might:
- have blood loss and need a blood transfusion
- get an infection
- have blood clots
- have a reaction to anaesthetic
- have damage to your bladder or bowel.
Vaginal and laparoscopic hysterectomies have lower risks of blood loss and infection when compared to an abdominal hysterectomy. Your specialist will explain the risks in more detail.
If you still have one or both ovaries after your hysterectomy, you might experience medically induced menopause or menopause that’s earlier than expected. So talk to your doctor if you have menopausal symptoms after the surgery.
If you have both ovaries removed during surgery, you will experience menopause straight away.
What happens after a hysterectomy?
Studies suggest that many women have improved symptoms after recovering from a hysterectomy. For example:
- reduced pelvic pain
- improved mood
- improved quality of life.
It may take up to 4 weeks to fully recover after a vaginal or laparoscopic hysterectomy and up to 6 weeks after an abdominal hysterectomy.
To learn more about recovering from a hysterectomy, visit the Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG) website.
Some women feel low or depressed after a hysterectomy for different reasons. Hormonal changes or feelings about an early end to your fertility may impact your mental health.
Know that you are not alone. Talk to people you trust and see your doctor if you are concerned.
Our review process
This information has been reviewed by clinical experts and is based on the latest evidence.
Our content review process ensures our health information is accurate, trustworthy, current and useful.
We regularly check our information to make sure it reflects the latest clinical guidelines and key findings from large, reliable studies.
Where possible, we focus on Australian research to make our information more relevant locally.
Experts play a key role in reviewing our content. Clinicians at Jean Hailes check information for accuracy and real‑world relevance. These include GPs, gynaecologists, endocrinologists, psychologists and allied health professionals.
We also work with partner organisations, independent specialists and people with lived experience to make sure our content reflects both expert knowledge and the experiences of the community.













