- About the menstrual cycle
- Phases of the menstrual cycle
- What is a period?
- Periods at different life stages
- What happens when you get your period?
- Period symptoms
- What can affect your periods?
- Health conditions related to your periods
- Sex during your periods
- When to see your doctor about your periods
- Period products
- Period pain
- Heavy periods
- Irregular periods
- Absent periods
- Premenstrual syndrome (PMS)
- Premenstrual dysphoric disorder (PMDD)
-
Reviewed
Key takeaways
- Periods are part of your body’s menstrual cycle. A period is when blood comes out of your vagina every cycle.
- Your periods can last from 3 to 7 days, but this may change at different life stages.
- Period pain happens when your uterus muscles tighten or cramp to push out the blood.
- See your doctor if your periods impact your quality of life, like your school, work and social life.
Sections on this page
- About the menstrual cycle
- Phases of the menstrual cycle
- What is a period?
- Periods at different life stages
- What happens when you get your period?
- Period symptoms
- What can affect your periods?
- Health conditions related to your periods
- Sex during your periods
- When to see your doctor about your periods
- Period products
- Period pain
- Heavy periods
- Irregular periods
- Absent periods
- Premenstrual syndrome (PMS)
- Premenstrual dysphoric disorder (PMDD)
Key takeaways
- Periods are part of your body’s menstrual cycle. A period is when blood comes out of your vagina every cycle.
- Your periods can last from 3 to 7 days, but this may change at different life stages.
- Period pain happens when your uterus muscles tighten or cramp to push out the blood.
- See your doctor if your periods impact your quality of life, like your school, work and social life.
About the menstrual cycle
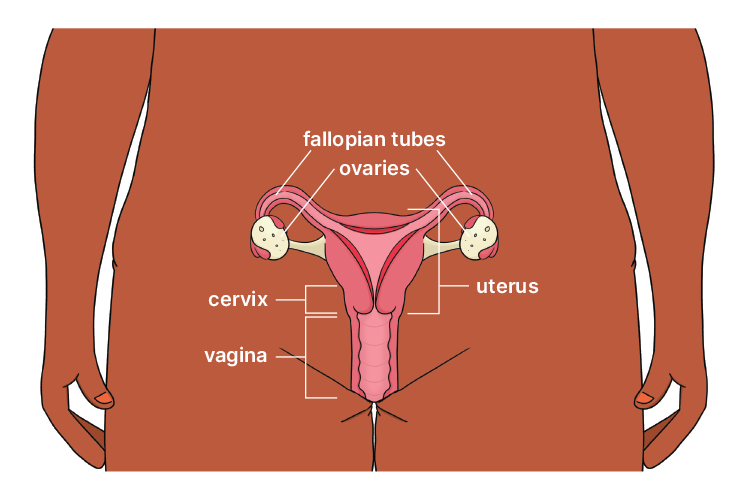
The menstrual cycle is a natural process in the female reproductive system. It repeats every cycle from your first period (menarche) to your final period menopause.
Each cycle begins on the first day of your period and ends the day before your next period.
When hormone levels change during your menstrual cycle, it can cause physical and emotional symptoms. You can better understand your menstrual cycle by keeping track of your periods and any symptoms you notice.
Phases of the menstrual cycle
The menstrual cycle has 4 phases: period, follicular phase, ovulation and luteal phase.
A period is when the lining of the uterus breaks down and leaves the body through the vagina. Periods contain blood, mucous and cells from the lining of the uterus.
This phase begins on the first day of your period and lasts until ovulation. It usually lasts for about 14 days. The lining of the uterus begins to thicken and small sacs (follicles) start to grow in the ovaries. One of these follicles grows into a mature egg.
Ovulation is when a mature egg is released from one of the ovaries. This usually happens every cycle, about 2 weeks before your next period starts.
A few days before ovulation, you might notice that the mucus in your vagina is thinner, clearer and more slippery. You might also feel pain in your lower belly, often on one side. This time is called ‘the fertile window’.
You are most likely to get pregnant if you have unprotected sex around the time of ovulation.
To avoid pregnancy, it’s important to use contraception throughout your cycle.
This phase begins after ovulation and ends before your next period. It’s when an egg moves towards the uterus. The body makes a hormone called progesterone to help prepare the uterus for a pregnancy. If the egg is fertilised by sperm, it can attach to the wall of the uterus and pregnancy begins. If the egg isn’t fertilised, you will get your period and a new cycle will begin.
The menstrual cycle is controlled by hormones. An average cycle is 28 days, but it can be shorter or longer.
Menstruation. The lining of the uterus breaks down and leaves the body. This bleed is also known as a period. Periods can last from 3 to 7 days.
Hormone levels rise, causing the lining of the uterus to start thickening in readiness for a possible pregnancy.
Ovulation. Around halfway through your cycle, an egg leaves an ovary and travels down the fallopian tube towards the uterus. This is when you are most likely to get pregnant.
If there is no pregnancy, hormone levels drop, the lining of the uterus breaks down and the menstrual cycle begins again.
The menstrual cycle is controlled by hormones. An average cycle is 28 days, but it can be shorter or longer.
End of transcript
Information about Jean Hailes for Women’s Health
Jean Hailes for Women’s Health is a national not-for-profit organisation dedicated to improving the health of all women, girls and gender-diverse people. For free, evidence-based and easy-to-understand health information, visit www.jeanhailes.org.au.
© 2024 Jean Hailes Foundation. All rights reserved. This publication may not be reproduced in whole or in part by any means without written permission of the copyright owner. Contact: licensing@jeanhailes.org.au
How long is an average menstrual cycle?
Everyone’s menstrual cycle is different, and it can change over time. When you first get your periods, your cycle may be longer and irregular. It can take 3 to 4 years for your periods to settle into a regular pattern. For adults, a normal cycle is usually between 24 and 38 days. The average length of a menstrual cycle is 28 days.
What is a period?
Periods are part of your body’s menstrual cycle. A period is when blood comes out of your vagina every cycle.
Periods at different life stages
In Australia, the average age to get your first period is 12 to 13, but it can start as early as 9 and as late as 16. It’s recommended you see a doctor if you haven’t had your first period by age 16.
Your final period is called menopause. In Australia, the average age to reach menopause is 51.
Your periods may change at different life stages. For example, it may be irregular in the lead-up to menopause (perimenopause).
What happens when you get your period?
Your periods might last from 3 to 7 days. Most people only lose a small amount of blood (33 mL on average).
At the start of your periods, the blood may be bright red and it may turn dark brown near the end.
It’s normal to see small blood clots, but if you see lots of clots or clots bigger than 3 cm in size, talk to your doctor.
You might have a small amount of blood (spotting) or pain around the time of ovulation. If this lasts longer than 3 days, it’s a good idea to see your doctor.
It’s normal for your periods to have a smell. Avoid using douches or perfumed soaps or sprays as these can cause vulval irritation.
Period symptoms
You may experience physical and emotional symptoms when you get your periods. For example:
- cramping
- bloating
- tender breasts
- irritability
- mood changes.
It’s important to rest and take time for yourself, especially if your energy or mood is low. If period-related symptoms stop you from doing normal activities, like school or work, see your doctor.
Symptoms experienced before your periods are called premenstrual syndrome or PMS.
What can affect your periods?
Many things can affect your periods, including your physical and emotional health and lifestyle.
Medicines and medical treatments can make your periods heavier, lighter or stop altogether. For example:
- copper intrauterine devices (IUDs) can cause heavier bleeding, longer periods and more painful periods
- hormone medicines (e.g. the Pill) can help regulate periods and reduce bleeding
- blood-thinning medicines can cause abnormally heavy periods
- some medicines, such as antipsychotics, can cause irregular or absent periods
- some medicines, such as anti-inflammatory drugs and tranexamic acid, can make periods lighter
- some cancer treatments can cause irregular or absent periods
- gender-affirming hormone medicine may cause irregular or absent periods.
Changing hormones, hormone conditions and hormone treatments can affect your periods. For example:
- changes in your periods
- changes in hormone levels at different life stages, such as after childbirth and during perimenopause, can cause
- thyroid problems can make your periods very light, heavy or irregular, or cause your periods to stop for several months.
Other factors can affect your periods. For example:
- regular physical activity can help reduce PMS symptoms and period pain
- high levels of stress or anxiety can contribute to PMS symptoms and irregular periods
- too much exercise can lead to absent periods (amenorrhoea)
- eating disorders, especially anorexia nervosa, can cause periods to stop
being overweight is associated with irregular cycles, absent periods, heavy bleeding and higher rates of PMS and PMDD - being unwell might make your periods late, or you may skip a period
- travel or big changes in routine can affect your periods.
Health conditions related to your periods
Some health conditions are associated with periods, so it’s important to see your doctor if you have symptoms such as painful periods or heavy periods.
Endometriosis
Endometriosis is a long-term condition where tissue, similar to the lining of the uterus, grows in other parts of your body.
Adenomyosis
Adenomyosis is a condition where tissue, similar to the lining of the uterus, grows in the muscle wall of the uterus.
Polycystic ovary syndrome (PCOS)
PCOS is a condition associated with increased levels of 2 hormones in the body: insulin and androgens (male-type hormones).
Premenstrual dysphoric disorder (PMDD)
PMDD is a serious health condition that causes severe emotional and psychological symptoms and distress one or 2 weeks before your periods.
Sex during your periods
You can have sex during your period, but it’s important to practise safer sex to stop the spread of sexually transmitted infections (STIs).
You should always use contraception if you don’t want to get pregnant.
When to see your doctor about your periods
There are many reasons why you might need to see a doctor about your periods. For example, if you have:
- heavy periods
- painful periods
- absent periods
- unusual bleeding (e.g. bleeding between periods, after having sex or after menopause).
Period products
There are many types of period products available, and the best choice depends on your comfort, lifestyle and preferences. This page explains the different options, how to use them safely, how often to change them, and how to dispose of them properly.
Period pain
Period pain is common and usually caused by the uterus tightening during your period, leading to cramping and discomfort in the pelvis, back or legs. This page explains what period pain is, what’s normal, possible causes, ways to manage it, and when to see your doctor.
Heavy periods
Heavy periods (heavy menstrual bleeding) are common and can significantly affect daily life when bleeding is heavier or lasts longer than usual. This page explains what heavy periods are, possible causes, treatment options, and when to see your doctor for support.
Irregular periods
Irregular periods are periods that don’t follow a typical cycle and can vary in timing, length or frequency. This page explains common causes of irregular periods, treatment options, and when to see your doctor for advice and support.
Absent periods
Absent periods (amenorrhoea) occur when you don’t get your periods at all, either temporarily or long term. This page explains the common causes, treatment options, and when to see your doctor if your periods haven’t started or stop unexpectedly.
Premenstrual syndrome (PMS)
Premenstrual syndrome (PMS) refers to the emotional and physical symptoms many people experience in the week or two before their period. This page explains common PMS symptoms, possible causes, ways to manage them, and when to see your doctor if symptoms affect daily life.
Premenstrual dysphoric disorder (PMDD)
Premenstrual dysphoric disorder (PMDD) is a severe condition that causes intense emotional and psychological symptoms in the one to two weeks before your period. This page explains how PMDD differs from PMS, common symptoms, treatment options, and when to see your doctor for support.
Our review process
This information has been reviewed by clinical experts and is based on the latest evidence.
Our content review process ensures our health information is accurate, trustworthy, current and useful.
We regularly check our information to make sure it reflects the latest clinical guidelines and key findings from large, reliable studies.
Where possible, we focus on Australian research to make our information more relevant locally.
Experts play a key role in reviewing our content. Clinicians at Jean Hailes check information for accuracy and real‑world relevance. These include GPs, gynaecologists, endocrinologists, psychologists and allied health professionals.
We also work with partner organisations, independent specialists and people with lived experience to make sure our content reflects both expert knowledge and the experiences of the community.
Want to learn about periods in your language?
Read our translated women’s health fact sheets that are written in plain language.




















