-
Reviewed
Key takeaways
- Common symptoms of adenomyosis include painful and heavy periods, and pelvic pain.
- Adenomyosis is different to endometriosis, but you can have both conditions at the same time.
- Treatments include hormone medicines and surgery.
- See your doctor if symptoms like painful periods impact your daily life.
Key takeaways
- Common symptoms of adenomyosis include painful and heavy periods, and pelvic pain.
- Adenomyosis is different to endometriosis, but you can have both conditions at the same time.
- Treatments include hormone medicines and surgery.
- See your doctor if symptoms like painful periods impact your daily life.
What is adenomyosis?
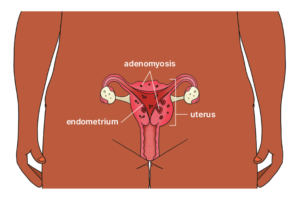
Adenomyosis is a condition where tissue, similar to the lining of the uterus, grows into the muscle wall of the uterus.
Adenomyosis only affects people who have periods, especially those aged 30 to 50. Studies suggest that about one in 5 women have adenomyosis.
Women with adenomyosis can also have endometriosis, but the conditions are different. With endometriosis, the tissue grows in other parts of your body, such as your fallopian tubes and ovaries.
How can adenomyosis affect periods?
With adenomyosis, the cells in your muscle wall bleed when you have your period. This can cause pain and other symptoms.
How can adenomyosis affect fertility?
Adenomyosis can cause fertility problems because the condition makes it hard for an embryo to implant into the lining of the uterus. Adenomyosis can also cause pregnancy complications. Ask your doctor for more information.
Symptoms of adenomyosis
If you have adenomyosis, you might not have any symptoms. But about 2 in 3 women with adenomyosis experience:
- painful periods
- heavy periods
- iron deficiency (anaemia) due to heavy periods, which can make you feel tired or dizzy
- painful sex (dyspareunia)
- persistent pelvic pain.
Causes of adenomyosis
We don’t know the exact cause of adenomyosis, but it may be associated with:
- surgery on the uterus
- cells in the muscle wall of the uterus before birth
- inflammation of the uterus lining after having a baby, making it easier for cells to pass into the muscle wall.
How is adenomyosis diagnosed?
Adenomyosis can be hard to diagnose because there are no agreed tests to confirm the condition. Adenomyosis can’t be diagnosed from blood tests or tissue samples (biopsies).
A diagnosis of adenomyosis is usually only confirmed after the uterus has been removed (hysterectomy).
If you think you might have adenomyosis, talk to your doctor. They will ask questions about your symptoms and may do a vaginal examination.
Your doctor might refer you to a gynaecologist. Depending on your situation, they may do an internal ultrasound via your vagina to help diagnose the condition.
You may also need to have a magnetic resonance imaging (MRI) scan. This technology can be used to rule out other conditions, such as fibroids, and help diagnose adenomyosis.
Treatments for adenomyosis
Treatment for adenomyosis will depend on your symptoms, stage of life and whether you plan to have children.
Research shows a commonly used IUD has the best outcomes for managing symptoms of adenomyosis.
A doctor or health care professional inserts the IUD into your uterus. It releases a hormone called progesterone, which reduces bleeding and pain and thins the endometrial cells. You can have the IUD removed if you are planning a pregnancy.
The Pill may reduce bleeding and pain, but research suggests it’s not as effective as an IUD. You can stop taking the Pill if you’re planning a pregnancy.
Talk to your doctor about the benefits and risks of each treatment option.
If you’re not planning any future pregnancies, you can have an operation to remove the uterus lining (endometrial ablation) to reduce heavy bleeding. This operation may not reduce pain. You can have an endometrial ablation and use an IUD to help with symptoms.
But if you are planning a pregnancy, your doctor or specialist may not recommend this surgery, as it can result in scar tissue that might affect your fertility.
If your symptoms are severe and you’re not planning to get pregnant, you can have surgery to remove your uterus (hysterectomy).
A non-surgical procedure called a uterine artery embolisation blocks blood supply to part of the uterus.
This procedure reduces pain and bleeding, but it’s not recommended if you’re planning future pregnancies.
You can use a natural approach in addition to the above treatments to help manage symptoms. For example:
- gentle physical activity
- meditation
- yoga
- acupuncture.
When to see your doctor about adenomyosis
Talk to your doctor if symptoms such as painful periods stop you from doing day-to-day activities.
Our review process
This information has been reviewed by clinical experts and is based on the latest evidence.
Our content review process ensures our health information is accurate, trustworthy, current and useful.
We regularly check our information to make sure it reflects the latest clinical guidelines and key findings from large, reliable studies.
Where possible, we focus on Australian research to make our information more relevant locally.
Experts play a key role in reviewing our content. Clinicians at Jean Hailes check information for accuracy and real‑world relevance. These include GPs, gynaecologists, endocrinologists, psychologists and allied health professionals.
We also work with partner organisations, independent specialists and people with lived experience to make sure our content reflects both expert knowledge and the experiences of the community.













