-
Reviewed
Key takeaways
- Many conditions can affect your vulva and vagina, but most improve with treatment.
- Thrush is a common infection of the vulva and vagina. Typical symptoms include itching, burning and vaginal discharge.
- Some conditions have similar symptoms to others, so it’s important to get the right diagnosis and treatment.
- See your doctor if symptoms last for a long time or come back after treatment.
Key takeaways
- Many conditions can affect your vulva and vagina, but most improve with treatment.
- Thrush is a common infection of the vulva and vagina. Typical symptoms include itching, burning and vaginal discharge.
- Some conditions have similar symptoms to others, so it’s important to get the right diagnosis and treatment.
- See your doctor if symptoms last for a long time or come back after treatment.
Vulval and vaginal thrush
Thrush is a common infection of the vulva and vagina, and sometimes the mouth. It’s also known as a yeast infection. Thrush affects 75% of women at least once in their lifetime.
Recurrent thrush
About 5% of women experience recurrent thrush. Recurrent thrush is when you have 4 or more episodes of thrush over one year. This is usually due to persistent infection rather than a new infection. But it may also be due to other health conditions, such as:
- iron deficiency
- diabetes
- immune disorders
- use of medicines, such as antibiotics.
If you think you have recurrent thrush, it’s important to see your doctor. They should investigate if your thrush is caused by other underlying conditions.
Typical symptoms of thrush include:
- an itchy vulva
- burning sensation of the vulva and vagina
- thick white vaginal discharge
- painful sex (dyspareunia)
- stinging when weeing
- swelling or redness of the vulva and vagina
- splits in the skin of the vulva.
Thrush is often caused by an overgrowth of candida in your vagina. Candida is a type of yeast.
It’s also thought that higher oestrogen levels can make women more likely to get thrush. Oestrogen increases the amount of sugar (glycogen) in your vagina, which creates a perfect environment for candida to grow and thrive.
Thrush is more likely to affect women who have periods, as they have higher levels of oestrogen. The condition is rare in girls who haven’t gone through puberty and in postmenopausal women (unless they are on oestrogen therapy).
You may also get thrush if you:
- take antibiotics
- take a higher-dose Pill
- use menopausal hormone therapy (MHT)
- use cortisone ointments
- are pregnant
- are about to have your period (due to hormone changes)
- have other health conditions, such as obesity, diabetes, iron deficiency or immune system disorders
- have vulval skin conditions, such as vulval psoriasis, lichen planus or lichen sclerosus.
When you see your doctor, they will ask about your symptoms and medical history. They should examine your vulva. They may also take a swab from your vagina (and vulva if it’s sore) and send it to a laboratory to see if candida is present.
Many women think an itchy vulva might be thrush and treat it with an over-the-counter medicine from the pharmacy. But it’s important to see your doctor for an accurate diagnosis, especially if over-the-counter medicine doesn’t work.
Most cases of thrush are treated with an antifungal cream or a vaginal pessary (tablet) that goes into your vagina.
Depending on the product and severity of symptoms, treatment time can range from one to 6 days. If you have mild symptoms, it may only take 3 days to treat.
If symptoms return, you may need a second course of treatment. It’s important to finish the full course of treatment – don’t stop when symptoms get better.
For recurrent thrush, your doctor might recommend:
- combined vaginal and oral antifungal medicine
- oral antifungal medicine to be taken regularly for up to 6 months
- a change in contraception
- a lower-oestrogen dose of MHT.
When you have thrush, sex can cause a burning feeling or pain. If this happens, you might want to avoid sex until your treatment has finished.
If you use condoms during sex, apply the thrush treatment cream after sex, as it can weaken condoms.
Thrush is not a sexually transmitted infection (STI), but it can be passed to a male sexual partner. This may cause a red or sore penis.
It’s important to take extra care of your vulva and other affected areas when managing this condition.
Untreated or recurring thrush can lead to ongoing vulval discomfort or painful sex. It may also lead to cracks or splits (fissures) in your vulva, which can become infected.
Thrush symptoms can be like those of other vaginal or vulval conditions. You should see your doctor if:
- you experience thrush-like symptoms for the first time
- you are unsure whether your symptoms are related to thrush
- your symptoms have not improved after treatment
- you continue to have painful sex after treatment.
- over-the-counter medicine has not improved symptoms
- you have recurring thrush
- you have thrush-like symptoms while you are pregnant or breastfeeding
- you have pain in your pelvic or vulval area
- you experience abnormal vaginal bleeding.
Bacterial vaginosis
Bacterial vaginosis is a bacterial infection of the vagina. Research shows that BV affects up to 30% of women at some stage in their life. Sexually active women of all ages can be affected.
More than half of all women with bacterial vaginosis (BV) do not have any symptoms. But some women may
- experience symptoms, such as:
- a watery, white, grey or greenish vaginal discharge
- an unpleasant or fishy smell
- discomfort and itching
- a burning sensation when weeing.
Bacterial vaginosis (BV) is caused by an overgrowth of bad bacteria in your vagina. Most cases are related to sexual activity, but other factors can increase your risk.
Women may be more likely to experience BV if they:
- have had multiple sexual partners during their lifetime
- have a new sexual partner
- practise unprotected sex
- practise douching, which enables bad bacteria to grow
- have a copper intrauterine device (IUD).
Your doctor will ask questions about your symptoms, medical history and sexual history, including details about past sexually transmitted infections (STIs).
They may:
- check your vagina
- take a vaginal swab to test for abnormal bacteria
- do a pH test to check the acidity of your vagina.
Bacterial vaginosis (BV) is usually treated with a course of antibiotics, taken as tablets or applied as vaginal cream or gel.
You’ll need to take the full course of antibiotics, even if symptoms go away before the end of the course. If you stop the treatment early, it could increase the risk of the infection coming back.
BV can reoccur with sexual contact, so avoid sexual activity until you have finished your antibiotics and your symptoms have gone. Research suggests that when a male partner is also treated, it may prevent the infection coming back.
BV can spread between female sexual partners. So, if your partner is female and you have been diagnosed with BV, encourage them to follow up with their doctor.
While treatment is usually effective, about 50% of women will have a recurrence of BV within 12 months. If symptoms return, visit your doctor for more treatment.
Safer sex practices, like using condoms, can protect against infection, regardless of your sexual partner’s gender.
Avoid using perfumed products in and around your vagina. For example:
- toilet paper
- tampons
- pads
- soaps and washes.
Don’t use douches as they may cause an imbalance in your vaginal bacteria. This can increase the risk of vaginal infection.
Bacterial vaginosis (BV) can increase the risk of:
- pregnancy and birth issues
- sexually transmitted infections (STIs), such as HIV, herpes, chlamydia or gonorrhoea
- infection after surgery (e.g. keyhole surgery via the belly, called a laparoscopy)
- pelvic inflammatory disease (PID) – an infection of the uterus, fallopian tubes and ovaries that can lead to infertility.
Bacterial vaginosis (BV) symptoms can be similar to those of other infections, so it’s important to get the right diagnosis and treatment. If you experience any BV symptoms, see your doctor.
Lichen planus
Lichen planus is an inflammatory skin condition triggered by the immune system. This condition affects about 1% of the population. It’s more common in women than men and it mainly affects adults aged 40 years and over. About 50% of people with the condition have it in their mouth.
Lichen planus is not contagious and can’t be spread through sex. It’s a lifelong condition that will need to be treated and monitored.
Lichen planus and lichen sclerosus can occur together.
Symptoms of lichen planus vary depending on the areas affected. When lichen planus affects the vulva and vagina, you may notice:
- lacy, white lesions on your vulva and at your vaginal opening
- reddish brown patches on the inner part of your vulva
- painful, burning sores in your vagina
- red, raw skin around your vulva
- scarring
- the sides of your vagina sticking together (adhesion).
You may also have:
- painful erosions and ulcerations
- severe itching
- painful vaginitis (inflammation of the vagina) with vaginal discharge
- vulval bleeding that happens easily on contact, especially after sex
- stinging when weeing
- painful sex (dyspareunia).
It’s thought that lichen planus is an autoimmune condition. These can cause the immune system to attack the body’s own tissues.
Other factors associated with lichen planus include:
- stress
- genetics
- injury to your skin (caused by scratching)
- hepatitis C
- viruses like those that cause chicken pox (herpes varicella) and shingles (herpes zoster)
- bacteria (Helicobacter pylori)
- vaccines and medicines.
Your doctor will ask about your symptoms and medical history. They will also ask to examine your vulva. They may take a small sample (biopsy) of vulval skin and send it to a laboratory for testing.
Depending on your situation, your doctor may refer you to a skin specialist (dermatologist) or gynaecologist who specialises in vulval conditions.
There is no cure for lichen planus, and you won’t be able to get rid of it completely. But treatment should reduce symptoms and stop the condition from getting worse.
Treatments may include:
- corticosteroid ointment applied on your vulva and in your vagina to reduce pain, itching and inflammation
- medicines and ointments to help reduce the body’s immune response
- surgery to remove scar tissue or adhesions that cover the entrance to your vagina – surgery is rare.
The ointments will:
- relieve symptoms
- reduce inflammation
- limit the risk of adhesion and scarring.
It’s important to use the ointments long-term and as prescribed. Your doctor will need to review this treatment regularly.
It’s important to take extra care of your vulva and vagina when managing this condition.
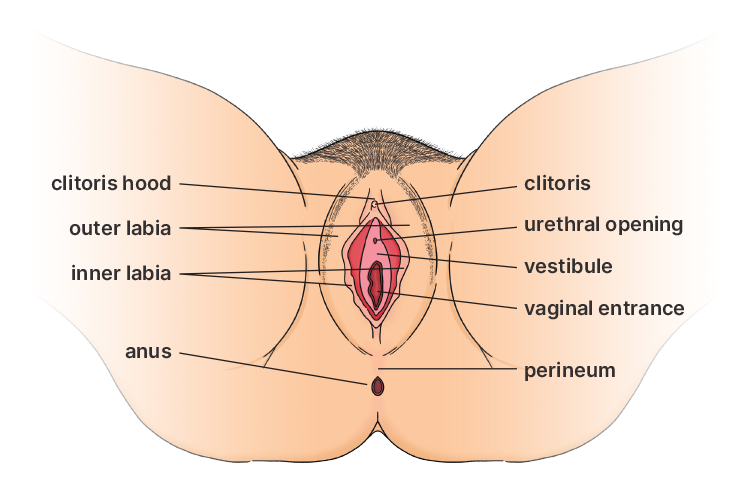
Lichen planus can lead to changes in your vulva and vagina, including:
- disappearance of your clitoral hood
- shrinkage of your inner lips (labia)
- your inner lips sticking together (adhesion)
- scarring that narrows your vaginal entrance.
Lichen planus doesn’t cause cancer, but it is associated with an increased risk of vulval cancer.
See your doctor if you notice any symptoms. It’s important to get the right diagnosis and treatment.
Sometimes lichen planus can be mistaken for other skin conditions, including lichen sclerosus.
If you are diagnosed with lichen planus, you’ll need to have regular, ongoing check-ups with your doctor to monitor your condition.
Lichen sclerosus
Lichen sclerosus is a chronic skin condition that usually affects the skin around your vulva and anus.
This lifelong condition is more common in women, particularly postmenopausal women.
It isn’t contagious and can’t be spread through sex. Lichen sclerosus and lichen planus can occur together.
Symptoms can range from mild to severe. People with a mild condition may not have any symptoms.
Lichen sclerosus can be in one small area or it can affect many areas, including the skin between your vagina and anus (perineum), inner lips (labia) and clitoral hood.
Common symptoms include:
- itchiness around your vulva or anal areas
- bruised or torn skin, blisters and ulcers (caused by scratching)
- cracked and bleeding skin
- pain or bleeding when doing a poo (caused by skin cracking or splitting)
- stinging when weeing
- painful sex (dyspareunia) due to skin splits at the vaginal opening.
The exact cause of lichen sclerosus is not known. But it’s thought to be an autoimmune condition. These conditions cause the immune system to attack the body’s own tissues.
About 15% of people with the condition have a family history of the disorder, so there may be a genetic link.
Lichen sclerosus is associated with other autoimmune conditions, such as:
- thyroid disease
- pernicious anaemia
- type 1 diabetes
- coeliac disease.
It can also co-exist with other skin conditions.
Lichen sclerosus is also associated with:
- hormonal imbalances (usually after menopause)
- previous damage to skin related to other skin conditions.
Your doctor will ask about your symptoms and medical history. They will also ask to examine your vulva. They may take a small sample (biopsy) of skin from around your vulva or anus and send it to a laboratory for testing.
It’s important for your doctor to examine the affected areas to ensure an accurate diagnosis.
There is no cure for lichen sclerosus, and you won’t be able to get rid of it completely. But treatment should reduce symptoms and stop the condition from getting worse.
The main treatment for lichen sclerosus is corticosteroid ointment. The ointment is applied to affected areas to:
- reduce pain, itching and inflammation
- stop the condition from getting worse.
Ointments are recommended instead of creams, as ointments are less likely to sting or cause contact dermatitis.
The ointment will relieve itching within a few days. But it will take some time for the skin to improve. After a few months, you may be able to reduce the frequency of treatment, but don’t stop unless your doctor tells you to.
This treatment is usually effective, but you will need regular check-ups with your doctor to monitor the condition.
Surgery may be needed to remove scar tissue that narrows the entrance to your vagina.
It’s important to take extra care of your vulva and other affected areas when managing this condition.
Lichen sclerosus can lead to changes in your vulva and other affected areas, including:
- small white spots that grow into larger white areas and may become wrinkled
- thickened patches of white skin with splits or fissures
- smooth white patches on your skin
- a buried clitoris due to your clitoris hood sticking together (adhesion)
- shrinkage of your inner lips (labia)
- tightening of your vaginal entrance.
Lichen sclerosus doesn’t cause cancer. But it is associated with an increased risk of vulval cancer, especially if the condition is left untreated.
See your doctor if you notice any symptoms. Sometimes lichen sclerosus can be mistaken for other skin conditions, including lichen planus, so it’s important to get the right diagnosis and treatment.
If you are diagnosed with lichen sclerosus, you will need to have regular, ongoing check-ups with your doctor to monitor your condition.
Vulvovaginal atrophy
Vulvovaginal atrophy is the thinning of your vaginal lining and vulval skin, caused by a drop in oestrogen levels around the time of menopause. Vaginal atrophy affects about 40% of postmenopausal women – and the risk increases with age.
This condition is also known as genitourinary syndrome of menopause (GSM), which includes vulvovaginal and urinary symptoms.
Symptoms of vulvovaginal atrophy include:
- dry vagina
- painful sex (dyspareunia)
- reduced vaginal lubrication during sex
- burning and itching in the vagina
- vulval irritation, especially when wearing tight pants or Lycra
- smelly vaginal discharge (sometimes mistaken for thrush)
- shortening and tightening of the vagina
- pale and thin labia and vagina
- reduced pubic hair
- spotting or light bleeding, including after sex – if this happens, see your doctor straight away.
Urinary symptoms include:
- frequent or urgent need to wee
- pain or burning sensation when weeing
- weeing more often than usual, including at night
- blood in your wee
- wee leakage (urinary incontinence)
- recurrent urinary tract infections (UTIs).
The vagina, and other tissues in the pelvis, need oestrogen to stay healthy. When oestrogen levels drop around the time of menopause, the tissues become drier, thinner and more fragile. This can increase the risk of irritation and UTIs.
Oestrogen levels may also decrease due to:
- breastfeeding
- medicine that reduces oestrogen levels, for example, the Pill
- medicine or surgery that causes medically induced menopause, for example, some cancer treatments, surgical
- removal of both ovaries and some hormone medicines.
Your doctor will ask about your symptoms and medical history. They will also ask to examine your vulva and vagina for signs of atrophy.
If you have discharge, your doctor may take a vaginal swab to check for infection.
If you have urinary symptoms, they may also order a urine (wee) test to check for a urinary tract infection (UTI).
Vulvovaginal atrophy is more likely to affect women over 50 or women who have gone through menopause. But other factors can increase your risk. For example, if you:
- have had your ovaries removed
- have had chemotherapy or radiation treatment
- are not sexually active – sex increases blood flow to the area and makes vaginal tissues more elastic
- have an immune disorder
- take medicines that affect oestrogen levels
- haven’t given birth vaginally
- smoke.
Depending on your situation, you may want to try hormonal treatments.
Vaginal oestrogens
Vaginal oestrogens are an effective treatment for vulvovaginal atrophy. They are available as creams, tablets and pessaries, which are inserted directly into the vagina.
This treatment improves blood flow in the pelvis and increases vaginal secretions.
Vaginal oestrogens will improve the health of your pelvic tissues, including your:
- vulva
- vagina
- bladder
- urethra
- pelvic floor muscles.
Menopausal hormone therapy (MHT)
MHT may improve vaginal symptoms and other menopausal symptoms, such as hot flushes and night sweats.
Hormone medicines may not be suitable if you have a history of oestrogen-receptor-positive cancer. Ask your doctor about the benefits and risks.
You can’t reverse vulvovaginal atrophy, but you can stop it from getting worse by seeking a diagnosis and starting treatment early.
Research suggests that MHT eliminates vulvovaginal atrophy symptoms in 75% of cases, while vaginal oestrogen therapy is effective in 80% to 90% of cases.
Without treatment, vulvovaginal atrophy may get worse over time.
It’s important to take extra care of your vulva and vagina when managing this condition.
You can try using a cold compress to help with itching and mild discomfort.
- Dilute half a teaspoon of bicarb soda in one litre of water.
- Soak a washcloth in the solution and apply it gently to your vulva a few times a day.
- Pat the area dry (instead of rubbing) afterwards.
You can also try:
- vaginal lubricants – to help with painful sex
- non-hormonal moisturisers – to help ‘plump up’ and add moisture to cells in your vagina
- regular sexual activity, including masturbation – to improve blood flow to your vagina
- adding flaxseed to your diet – to help with vaginal dryness
Many women have symptoms of vulvovaginal atrophy, such as painful sex. But they don’t seek treatment because they feel embarrassed or think nothing can be done.
It’s important to get the right diagnosis and treatment, so see your doctor if you have any symptoms.
Vaginismus
Vaginismus is when your pelvic floor muscles involuntarily tighten. This can happen before or during an attempt to insert something into your vagina. For example:
- before or during sex
- when inserting a tampon or sex toy
- during a vaginal examination.
There are 2 types of vaginismus:
- Primary – where vaginal penetration has never been achieved.
- Secondary – where vaginal penetration was possible but is no longer possible for different reasons.
The main symptom of vaginismus is the involuntary tightening of your pelvic floor muscles in the lower part of your vagina. This can cause symptoms of pain and discomfort with any attempted vaginal penetration.
Vaginismus can occur for many reasons. It may be associated with physical factors, such as:
- medical conditions, for example, recurrent urinary tract infections (UTIs), thrush, persistent pain syndromes, endometriosis
- sexually transmitted infections (STIs) and ongoing pain after an STI has been treated
- vulval skin conditions, for example, lichen sclerosus and lichen planus
- vulval pain, including changes to the vulval skin and lining of the vagina, which happens at menopause.
Psychological factors may play a role. For example, fear due to trauma during childbirth or surgery, or negative ideas about sex.
Fear may also be due to previous experience of:
- painful vaginal examinations
- painful sex (dyspareunia)
- sexual assault or rape.
Other psychological factors may include:
- anxiety
- depression
- relationship problems
- feeling self-conscious
- fear of intimacy
- fear of pregnancy
- lack of arousal.
Vaginismus can cause some women to avoid situations where attempts at vaginal penetration might occur. For example:
- dating
- sex
- pelvic examinations.
Past experiences of pain can set up a cycle of fear of pain and muscle contraction.
Vaginismus is usually diagnosed via a clinical examination. During your first visit, your doctor will ask about your symptoms and medical, family and sexual history. They may also ask about sexual trauma and abuse.
If your doctor suspects vaginismus, they may ask to do a gentle physical examination, although this may not be possible.
Your doctor or specialist will recommend different treatment options depending on your individual situation. Common treatments include:
- pelvic floor physiotherapy, for example, pelvic floor muscle relaxation exercises, gentle massage, equipment such as biofeedback and vaginal trainers
- counselling
- medicine to help with any persistent pain issues.
If you have any concerns about your vulva or vagina, talk to your doctor. They might refer you to other specialists, for example:
- a pelvic floor physiotherapist
- a counsellor or psychologist
- a sex therapist.
Personal stories about vulval and vaginal health
Our review process
This information has been reviewed by clinical experts and is based on the latest evidence.
Our content review process ensures our health information is accurate, trustworthy, current and useful.
We regularly check our information to make sure it reflects the latest clinical guidelines and key findings from large, reliable studies.
Where possible, we focus on Australian research to make our information more relevant locally.
Experts play a key role in reviewing our content. Clinicians at Jean Hailes check information for accuracy and real‑world relevance. These include GPs, gynaecologists, endocrinologists, psychologists and allied health professionals.
We also work with partner organisations, independent specialists and people with lived experience to make sure our content reflects both expert knowledge and the experiences of the community.

Health information in your language
You might want to know more about

Gynaecological cancers


















