-
Reviewed
Key takeaways
- Fibroids are very common in women under the age of 50.
- They can cause heavy periods, painful periods and irregular bleeding.
- If symptoms don’t impact your daily life, you can leave them untreated.
- See your doctor if you have very heavy periods or a sudden change to your bleeding.
Key takeaways
- Fibroids are very common in women under the age of 50.
- They can cause heavy periods, painful periods and irregular bleeding.
- If symptoms don’t impact your daily life, you can leave them untreated.
- See your doctor if you have very heavy periods or a sudden change to your bleeding.
What are fibroids?
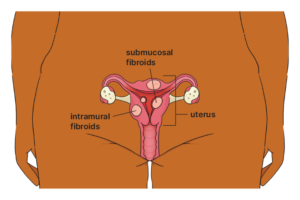
Fibroids are noncancerous growths found in the muscle wall of the uterus. They can vary in size from a pea to a rockmelon or even bigger.
Fibroids can grow:
- on the outer wall of the muscle (subserosal)
- within the muscle wall (intramural)
- on the inner wall lining the cavity of the uterus (submucosal).
- Up to 70% of women aged under the age of 50 have fibroids. After menopause, fibroids usually shrink and may even disappear.
How can fibroids affect fertility?
Fibroids can cause fertility problems, depending on their size and location. They can also cause pregnancy complications.
If you have fibroids and are planning a pregnancy, talk to your doctor about treatment options.
Symptoms of fibroids
Some people who have fibroids don’t experience symptoms. But 20% to 30% of women experience symptoms such as:
- heavy periods or longer periods than normal
- painful periods
- bleeding in between periods – this depends on the size and position of the fibroids
- iron deficiency (anaemia), due to heavy periods, which can make you feel tired or dizzy
- painful sex (dyspareunia)
- feeling heaviness or pressure in your back, bowel or bladder
- feeling like you haven’t emptied your bowel or bladder
- weeing a lot
- swelling in your lower abdomen.
Causes of fibroids
We don’t know exactly what causes fibroids, but we do know the female hormones oestrogen and progesterone stimulate the growth of fibroids.
Many risk factors for fibroids can’t be changed, such as your family history, health conditions like PCOS and when your first periods started. But you can reduce your risk by working with a doctor to maintain a healthy weight range and reduce your blood pressure.
How are fibroids diagnosed?
If you think you might have fibroids, talk to your doctor. They will ask questions about your symptoms and might recommend a scan or procedure to confirm the diagnosis.
Fibroids can be diagnosed in different ways. For example:
- an external ultrasound on your belly (abdomen)
- an internal ultrasound via the vagina
- a magnetic resonance imaging (MRI) scan
- a hysteroscopy – a thin telescope that shows the inside of your uterus
- a laparoscopy – a thin telescope that goes into your belly button to see your pelvic organs (performed under general anaesthetic).
Treatments for fibroids
Most fibroids don’t need treatment, unless:
- you’re planning to get pregnant
- your symptoms stop you from doing things you normally do.
If fibroids don’t affect your daily life, you can choose to leave them untreated.
Your doctor may recommend different medicines to treat your fibroids. For example:
- mefenamic acid tablets
- tranexamic acid tablets
- hormone medicines, such as the Pill or an IUD.
If fertility is an issue, your doctor might suggest a combination of medicines to shrink your fibroids. Ask them about the benefits and risks of each medicine.
Fibroids can grow back after you stop treatment.
You may be able to treat your fibroids with radiological treatment. For example:
- a non-surgical procedure called uterine artery embolisation that blocks blood supply to part of the uterus
- ultrasound guided by magnetic resonance imaging (MRI) – only suitable for certain types of fibroids.
You may need surgery to remove your fibroids. The type of surgery will depend on the size and position of your fibroids. Ask your doctor or specialist for more information.
When to see your doctor about fibroids
See your doctor if you experience symptoms such as:
- a sudden change to your bleeding
- very heavy periods (i.e. soaked pads every hour or large blood clots)
- unexplained weight loss or loss of appetite.
Our review process
This information has been reviewed by clinical experts and is based on the latest evidence.
Our content review process ensures our health information is accurate, trustworthy, current and useful.
We regularly check our information to make sure it reflects the latest clinical guidelines and key findings from large, reliable studies.
Where possible, we focus on Australian research to make our information more relevant locally.
Experts play a key role in reviewing our content. Clinicians at Jean Hailes check information for accuracy and real‑world relevance. These include GPs, gynaecologists, endocrinologists, psychologists and allied health professionals.
We also work with partner organisations, independent specialists and people with lived experience to make sure our content reflects both expert knowledge and the experiences of the community.













