- What is persistent pelvic pain?
- What does persistent pelvic pain feel like?
- When does pelvic pain happen?
- Why is some pain persistent?
- How can persistent pelvic pain affect you?
- How health conditions can impact pelvic pain
- How mental health can impact pelvic pain
- How social connections and work can impact pelvic pain
- How to get help for pelvic pain
- A person-centred approach for persistent pelvic pain
- Your health care team for persistent pelvic pain
- Medicine to help manage your pain
- How long will it take to reduce your pelvic pain?
- Physical activity to manage persistent pelvic pain
- Eat well to reduce pain
- Good bowel habits to reduce pain
- Look after your mental health to reduce pain
- Practical ways to manage your persistent pelvic pain
- Online and app resources
-
Reviewed
Key takeaways
- Persistent pelvic pain is pain in your pelvic area that is felt most days and lasts for more than 6 months.
- Pelvic pain is impacted by physical health conditions, like endometriosis, and other factors, such as stress and social connection.
- Persistent pelvic pain is best managed by a team of health care professionals, such as doctors, gynaecologists, pelvic floor physiotherapists and psychologists.
- Treatments include medicine, physiotherapy and lifestyle changes.
Sections on this page
- What is persistent pelvic pain?
- What does persistent pelvic pain feel like?
- When does pelvic pain happen?
- Why is some pain persistent?
- How can persistent pelvic pain affect you?
- How health conditions can impact pelvic pain
- How mental health can impact pelvic pain
- How social connections and work can impact pelvic pain
- How to get help for pelvic pain
- A person-centred approach for persistent pelvic pain
- Your health care team for persistent pelvic pain
- Medicine to help manage your pain
- How long will it take to reduce your pelvic pain?
- Physical activity to manage persistent pelvic pain
- Eat well to reduce pain
- Good bowel habits to reduce pain
- Look after your mental health to reduce pain
- Practical ways to manage your persistent pelvic pain
- Online and app resources
Key takeaways
- Persistent pelvic pain is pain in your pelvic area that is felt most days and lasts for more than 6 months.
- Pelvic pain is impacted by physical health conditions, like endometriosis, and other factors, such as stress and social connection.
- Persistent pelvic pain is best managed by a team of health care professionals, such as doctors, gynaecologists, pelvic floor physiotherapists and psychologists.
- Treatments include medicine, physiotherapy and lifestyle changes.
What is persistent pelvic pain?
Persistent pelvic pain (PPP) is pain in your pelvis, or lower abdomen, that is felt most days and lasts for more than 6 months.
Sometimes the pain is a symptom of other conditions, such as endometriosis, but it can be a condition of its own.
Persistent pelvic pain is complex and can be influenced by many things. For example:
- health conditions
- sleep quality
- mood
- work environment.
Persistent pelvic pain is quite common. It affects about one in 4 women and may be even more common in young women.
What does persistent pelvic pain feel like?
Persistent pelvic pain affects everyone differently. Your pain may be steady, or it may come and go. And the type of pain can change.
You may experience:
- a dull pelvic ache
- sharp, stabbing pain in the pelvis
- painful pelvic cramps
- pain in your pubic bone
- pain across your pelvis
- pressure or heaviness in your pelvis
- tingling or ‘pins and needles’ in your pelvis
- sensitivity in your lower abdomen.
When does pelvic pain happen?
You may experience pelvic pain at any time or at specific times, such as:
- during sex
- when using tampons
- during your period
- when going to the toilet
- when sitting or standing for long periods of time
- when you do certain movements or activities.
Why is some pain persistent?
Your pain might start because of:
- a health condition
- your periods
- an injury.
It may also be influenced by factors, such as stress or poor sleep.
Over time, the pain can cause changes to your muscles, nervous system and other tissues, leading to persistent pain.
How can persistent pelvic pain affect you?
Living with persistent pelvic pain can affect your life in many ways.
It can cause changes in various organs and muscles, which may lead to other physical problems. For example, changes in certain muscles can lead to bladder and bowel problems.
Persistent pelvic pain can affect your quality of life. For example, your:
- work
- sleep
- sex life
- personal relationships
- social life
- mental health.
How health conditions can impact pelvic pain
Period pain is when your uterus muscles tighten at the start of your periods. This pain can contribute to persistent pelvic pain.
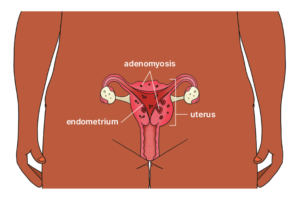
Endometriosis is a condition where tissue, similar to the lining of the uterus, grows in other parts of your body. Pain is a common symptom of endometriosis, which can contribute to persistent pelvic pain.
Adenomyosis is a condition where tissue, similar to the lining of the uterus, grows in the muscle wall of your uterus. Painful periods are a common symptom of adenomyosis, which can contribute to persistent pelvic pain.
Irritable bowel syndrome (IBS) is a group of symptoms, such as bloating and pain in your pelvic area, which can contribute to persistent pelvic pain.
Your pelvic floor muscles are part of a group of muscles called your core. Tight pelvic floor muscles can cause painful sex and pelvic pain, which can contribute to persistent pelvic pain.
Painful bladder syndrome is a condition where you have bladder pain and a frequent and urgent need to wee. Symptoms, such as tenderness in the pelvic area, can contribute to persistent pelvic pain.
A urinary tract infection (UTI) is an infection that affects the urinary system, including the bladder, urethra and kidneys. Symptoms, such as pain in your lower belly when doing a wee, can contribute to persistent pelvic pain.
Vulvodynia is the medical term for chronic pain or discomfort in the vulva that lasts for at least 3 months. With this condition, any pressure applied to the vulva, such as having sex, can contribute to persistent pelvic pain.
Chronic pelvic pain syndrome is when you have persistent pelvic pain without an underlying physical health condition.
How mental health can impact pelvic pain
Stress activates your nervous, hormone and immune systems, which causes changes in your body and brain. These changes can affect you physically and psychologically, which can contribute to persistent pelvic pain.
Poor sleep can increase the likelihood of pain and pain sensitivity. And pain can affect the quality and duration of your sleep. Disturbed sleep is also linked to depression and anxiety, which are more common with persistent pelvic pain.
Traumatic experiences, such as sexual assault and abuse, can contribute to persistent pelvic pain.
The way you think about pain can influence the way your body responds and how you cope with it. If your nervous system is overly sensitive, even thinking about pain can make you feel pain.
Being on high alert for pain may also intensify your pain experience.
How social connections and work can impact pelvic pain
If you live with persistent pelvic pain, it can be hard to connect with others. This may cause you to withdraw and have fewer social contacts. But social isolation is associated with anxiety and depression, which can influence persistent pelvic pain.
Your work environment can contribute to persistent pelvic pain. Poor job satisfaction, an unhappy workplace and lack of support from employers also linked to increased pain.
How to get help for pelvic pain
Everyone’s experience of persistent pelvic pain is different. For some, pain gets better without treatment. Others need to work at reducing their pain over time.
If you see a doctor about your pain, book a long appointment so you have time to talk about potential causes and pain management options. You can also bring a support person, like a friend or family member, to your appointment if you need one.
It can take time to get a diagnosis of persistent pelvic pain. Depending on your symptoms, your doctor may refer you to different health care professionals.
It’s important to give your doctor as much information about your pain as possible. This will help them to investigate potential causes.
It’s a good idea to bring:
- your medical records, including your past medical history
- blood test results
- X-rays and other scans, such as pelvic ultrasound reports
- information about previous surgeries.
It’s also helpful to keep a record or pain diary, and bring it with you to your appointment.
Keep track of important details, such as:
- when you have pain
- where you feel pain
- how the pain affects you
- what the pain feels like (sharp, cramping, dull ache)
- anything that makes the pain worse
- things you’ve tried to help manage your pain, like heat packs.
Your doctor may ask questions about your pain and how it affects your life. For example:
- How and when did your pain begin?
- How long does your pain last?
- How does your menstrual cycle affect your pain?
- Does your pain affect your sleep?
- Has your pain spread or become worse since it began?
They may also ask:
- Do you have pain when going to the toilet?
- Does the pain affect your mood?
- Which medicines have you used in the past? Have they helped?
- Which medicines or supplements are you taking now?
- Does your pain affect your daily life, such as work, study and social activities?
- Does your pain affect your relationships or sex life?
Your doctor may ask to do a physical examination to check:
- your posture and the way you walk and move (gait) – this may suggest pelvic muscle pain
- your lower back, hips, tailbone (coccyx) and pelvic joints – this is often associated with pelvic muscle dysfunction
- your lower abdomen – for lumps or tender points
- your vulva and vagina
- your pelvic floor muscles
- your skin – to see if you have a skin condition, numbness or tenderness.
You may need tests and procedures to check for other causes of pain, such as:
- blood or urine (wee) tests
- swabs to check for sexually transmitted infections (STIs), bacteria or other infections
- a cervical screening test
- imaging tests, such as an abdominal X-ray, ultrasound, CT scan or MRI scan of your abdomen and pelvis
- keyhole surgery to check your internal organs, such as your uterus or stomach
- a procedure to examine your bladder called a cystoscopy.
It’s important to ask questions and learn as much as possible about persistent pelvic pain. These questions may also help you find the best doctor to treat your pain.
You can ask:
- What experience do you have in managing persistent pelvic pain?
- Do you work with other health professionals to manage persistent pelvic pain?
- Which other health professionals should I see for my pain?
- Which tests will I need?
- How much will the tests cost?
- Where can I have these tests?
You can also ask:
- What kinds of treatments are available and how much do they cost?
- Are there any potential side effects?
- What practical things can I do to help manage my pain?
- Can you recommend any resources to learn more about my condition?
- Can I access any programs that make it more affordable to see different health professionals? For example, a GP
- Chronic Condition Management Plan or Mental Health Care Plan.
It’s a complex process to diagnose and manage persistent pelvic pain.
Your doctor might:
- refer you to one or more health care professionals
- suggest you try different medical and non-medical treatments to help manage your pain
- organise other tests (e.g. an ultrasound).
A person-centred approach for persistent pelvic pain
Persistent pelvic pain is a complex condition that’s influenced by health conditions, mental health and social factors.
Everyone has a different experience, which is why treatment should be person-centred.
Your treatment plan should focus on managing symptoms that bother you. It might include one or more of the following:
- pain education
- lifestyle changes, including diet, physical activity and sleep
- psychotherapy, such as cognitive behavioural therapy (CBT), relaxation and mindfulness techniques
- pelvic floor physiotherapy
- pain-relief medicine
- hormone medicines
- complementary therapies, such as acupuncture
- surgery for conditions like endometriosis (if other treatments haven’t worked).
Your health care team for persistent pelvic pain
Persistent pelvic pain is best managed by a team of health care professionals. But it can be hard to find the right help, especially in regional and remote areas.
You can ask your doctor to help you find local specialists or specialists who offer Telehealth appointments.
Depending on your situation, you might see different health care professionals.
Your doctor will provide most of your care and will start your treatment.
They will refer you to specialists and coordinate care with the rest of your health care team. They will also continue to manage your overall health.
A gynaecologist is a specialist in the female reproductive system.
They can diagnose and treat conditions like endometriosis, adenomyosis, fibroids and complex period problems.
Pain specialists are medical doctors with advanced training in pain management.
They understand the complex nature of pain and use different approaches to help reduce your pain.
Pelvic floor physiotherapy is widely used to manage persistent pelvic pain. Pelvic floor physiotherapists have extra training and special skills in women’s health.
They can:
- help improve how your pelvic floor and abdominal muscles, back and hips work
- help you learn how to move and exercise in a way that’s right for you
- help you learn about pain, which is an important part of managing pain
- explain basic pain-relief techniques.
Psychologists may use a range of techniques, including cognitive behavioural therapy (CBT) to help manage your pain.
They can:
- help you understand how your thoughts, emotions, physical sensations, behaviours and pain are linked
- recommend coping strategies to help manage your pain
- help with anxiety and depression, which are common in people with persistent pelvic pain.
Sex therapists can help you understand how persistent pelvic pain might cause painful sex.
Past experiences of painful sex may cause you to fear pain. This fear can create stress, tension and reduced sex drive and arousal.
If you want to improve your sexual experience, it may help to discuss your feelings with a sex therapist.
Dietitians can help you identify food that might trigger a pain flare. They can also recommend a balanced diet to help reduce your pain.
Naturopaths can provide complementary ways to manage your pain, including:
- supplements
- herbal medicine
- acupuncture
- lifestyle changes.
Many women use these therapies to manage their health, but there is limited evidence to support their safe and effective use.
If you’re using complementary therapies to manage your pain, it’s important to discuss the benefits and risks with your doctor.
Urogynaecologists are specialists in pelvic health.
They can diagnose and treat bladder and pelvic floor problems that may contribute to pelvic pain.
Gastroenterologists specialise in conditions that affect the digestive system.
They can diagnose and treat digestive conditions that may be causing pain.
Sleep specialists are doctors who diagnose and treat sleep disorders.
They can help with medicines and sleep routines to improve the quality of your sleep.
Your women’s health care team – Easy Read
Learn about different healthcare professionals and how they can help.
Medicine to help manage your pain
Medicine can be used to help manage persistent pelvic pain. While this may be useful, it should only be one part of your treatment plan.
Your health care team may recommend short-term pain-relief medicine, such as:
- paracetamol
- ibuprofen
- naproxen.
These may be useful for certain types of persistent pelvic pain, for example, period pain.
Health care professionals may also suggest medicines that target nerve pain, or hormone medicines, such as:
- the Pill
- an intrauterine device (IUD)
- hormone injections.
Opioids (strong pain-relief drugs) are not recommended for persistent pelvic pain as they can make the pain worse and might lead to dependency with regular use.
How long will it take to reduce your pelvic pain?
It may take time and different approaches to reduce your pelvic pain. It can take 3 to 6 months for your treatment to start working.
During this time, it’s important to be patient and follow your plan, even if you don’t notice any difference straight away.
Successful treatment may not get rid of your pain completely, but it will help you manage pain in the future.
Physical activity to manage persistent pelvic pain
Physical activity is an important part of staying healthy. But many people who have persistent pelvic pain avoid moving, as they fear it will make their pain worse.
Low-impact activities, such as swimming and walking can help to reduce your pain sensitivity.
Talk to your health care team about a tailored physical activity plan.
Some mind-body practices, such as yoga and stretching, can help you manage pelvic pain.
Pelvic pain can lead to tense muscles, especially:
- pelvic floor muscles
- abdominal muscles
- hip muscles.
When your muscles stay tight, you can have painful muscle cramps.
A pelvic floor physiotherapist can help you relax your pelvic floor muscles and stretch your stomach and the muscles on the outside of your pelvis.
These exercises may reduce pain and improve your bladder, bowel and sexual function.
For easy stretches to relax the pelvis, visit the Pelvic Pain Foundation of Australia website.
Guided-relaxation exercises and yoga can reduce tension in other areas of your body, which may also reduce pelvic pain.
Pacing means you do enough exercise to improve your pain without causing a pain flare. It’s a fine balance – and it may take time to learn your limits.
It can be helpful to keep track of your activities and responses to see if you can find where your limits are. By pacing, you gradually build your strength while staying within your comfort zone.
Why activity pacing matters
Many people with persistent pelvic pain experience higher pain sensitivity and fatigue after activity. Pacing helps to prevent these flare-ups.
By learning to listen to your body and understanding your limits, you can avoid the frustration of setbacks. Over time, consistent pacing can help you improve your:
- fitness
- confidence
- quality of life.
How to pace your activity and find your baseline
- Choose the type of activity you want to do.
- Track how much activity you can do without having a pain flare.
- Record 3 days of activity (they don’t have to be consecutive days).
- You can record your activity in different ways (minutes, distance or repetitions).
- Work out the average amount of activity you can do without a pain flare. This is your ‘baseline’.
- Work out your ‘starting point’ by reducing your baseline by 20%. This encourages you to move, even on bad days.
- Gradually increase your activity by 10% each week.
Example
Activity: walking.
- Day 1: 20 minutes
- Day 2: 30 minutes
- Day 3: 25 minutes
- Total: 75 minutes
Baseline: 25 minutes (total divided by 3)
Starting point: 20 minutes (baseline minus 20%)
Use the example above to find your baseline and starting point.
Track your activity
It’s important to keep track of your activities and how you feel afterwards. You can use a journal, a spreadsheet or an app on your phone.
Record:
- the activity you did
- when you did it
- the minutes, distance or repetitions you did
- how much rest you had
- how you felt during and after the activity (e.g. pain and fatigue levels).
Helpful tips
- Focus on activities you want to do.
- Start with smaller, easier activities.
- Schedule pacing into your day.
- Have planned rest breaks.Try to stick to your plan.
If you’re having a difficult day, you can:
- try to stay active, but take more rest breaks
- reduce your activity if you need to.
Things to remember
- If you’re having a good day, don’t be tempted to do more.
- If your activity is getting easier, or you want to try a new activity, work out a new baseline and starting point.
- It’s normal to have sore muscles for a day or so after doing a new or more challenging activity. This will reduce as your muscles get stronger. This is not a pain flare.
Don’t be concerned about mild discomfort that goes away about 30 minutes after the activity. This is not a pain flare.
While you’re learning how to pace yourself, it can be helpful to work with:
- a pelvic floor physiotherapist
- an exercise physiologist.
Eat well to reduce pain
The food you eat may influence your persistent pelvic pain.
Research suggests an anti-inflammatory diet can help reduce persistent pain. Read more about the anti-inflammatory diet on the Arthritis Movement website.
A dietitian can help you develop a nutrition plan. This may be helpful if you have a condition that’s impacted by the food you eat, such as:
- irritable bowel syndrome (IBS)
- painful bladder syndrome.
Good bowel habits to reduce pain
Good bowel habits are important if you have persistent pelvic pain, especially if you have irritable bowel syndrome (IBS).
Look after your mental health to reduce pain
Persistent pelvic pain can affect your mental health. It can cause:
- stress
- anxiety
- depression
- sleep problems
- sexual problems
- strained relationships.
Looking after your mental health can make it easier to manage pain. You can ask your doctor for a referral to a psychologist.
When you’re stressed, your body releases chemicals that are similar to the ones released when you feel pain.
These chemicals can turn up the volume of your pain. Stress management is an important part of managing persistent pelvic pain.
Learn more about looking after your mental health on the Beyond Blue website.
It can be hard to get a good night’s sleep when you have persistent pelvic pain, but there are practical things you can do to improve your sleep and quality of life.
For more information about sleep, visit the Sleep Health Foundation website.
Persistent pelvic pain can make you feel emotionally drained and withdrawn. It’s important to seek support from people close to you.
Talking to friends or family about your pain can be helpful. Find ways to connect that work for you, like a walk or phone call.
If you have a partner, they might not understand what you’re going through. You can tell them about your pain, what causes it and what makes it better.
If your pain is affecting your sex life, try to communicate openly with one another. It may also help to speak to a psychologist, sex therapist or relationship counsellor.
Practical ways to manage your persistent pelvic pain
Warm baths and heat packs can provide relief from cramping and muscle spasms.
Massage therapy can relieve tightness and pain in soft tissues.
Research suggests that massage can help you become more aware of your body and where you hold tension. This awareness can support changes that reduce muscle tightness, lower stress and reduce pain.
Deep breathing (belly breathing) brings more oxygen into your body and slows your heart rate. It can help you relax your pelvic floor muscles and other muscles in your body.
When you focus on your breath, it can distract you from unhelpful thoughts and sensations such as pain.
How to deep breathe
- Find a quiet, comfortable place to sit or lie.
- Breathe in slowly through your nose.
- Allow your chest and lower belly to rise while you breathe in.
- Let your belly fully expand as it fills with air.
- Slowly breathe out through your mouth.
You can also focus on calming images or a word that helps you relax while you practise your deep breathing.
A TENS machine is a small, battery-operated device with sticky pads (electrodes) that are attached to your skin. When the machine is turned on, it sends small electrical impulses, which causes a tingling feeling.
A TENS machine:
- changes the signals that go to the spinal cord and brain
- helps the body release endorphins, which are the body’s natural pain relievers.
Learn more about TENS on the Healthdirect website.
Online and app resources
These websites may help you learn more about pain and coping strategies:
- Pelvic Pain Foundation of Australia: information for women and People Assigned Female at Birth
- Pelvic Pain Foundation of Australia: Introduction to Pelvic Pain by Dr Susan Evans
You can also try these online programs and apps for pain:
Our review process
This information has been reviewed by clinical experts and is based on the latest evidence.
Our content review process ensures our health information is accurate, trustworthy, current and useful.
We regularly check our information to make sure it reflects the latest clinical guidelines and key findings from large, reliable studies.
Where possible, we focus on Australian research to make our information more relevant locally.
Experts play a key role in reviewing our content. Clinicians at Jean Hailes check information for accuracy and real‑world relevance. These include GPs, gynaecologists, endocrinologists, psychologists and allied health professionals.
We also work with partner organisations, independent specialists and people with lived experience to make sure our content reflects both expert knowledge and the experiences of the community.
Want to learn about pelvic pain?
The Jean Hailes ‘Pelvic Pain in Australian Women report’ from 2023 showed that 47% of Australian women have experienced pelvic pain in the last 5 years. But only half of them discussed their symptoms with a doctor.
You might want to know more about

Bladder health