- How your bowel works
- How your pelvic floor supports your bowel
- How to have good bowel health
- What’s normal?
- What’s not normal?
- How your gut affects bowel health
- How to improve your gut health
- Bowel cancer screening
- What is bowel incontinence?
- How to get a diagnosis of bowel incontinence
- Prevention and management of bowel incontinence
- Understanding irritable bowel syndrome (IBS)
- Symptoms of IBS
- Causes of IBS
- How to get a diagnosis of IBS
- Treatment and management of IBS
-
Reviewed
Key takeaways
- Signs of a healthy bowel include doing regular, soft, formed poos and going to the toilet without straining or a sense of urgency.
- Bowel cancer screening can reduce your risk of illness or death from cancer.
- See your doctor if you notice blood in your poo, ongoing constipation or diarrhoea, or unexplained weight loss.
Sections on this page
- How your bowel works
- How your pelvic floor supports your bowel
- How to have good bowel health
- What’s normal?
- What’s not normal?
- How your gut affects bowel health
- How to improve your gut health
- Bowel cancer screening
- What is bowel incontinence?
- How to get a diagnosis of bowel incontinence
- Prevention and management of bowel incontinence
- Understanding irritable bowel syndrome (IBS)
- Symptoms of IBS
- Causes of IBS
- How to get a diagnosis of IBS
- Treatment and management of IBS
Key takeaways
- Signs of a healthy bowel include doing regular, soft, formed poos and going to the toilet without straining or a sense of urgency.
- Bowel cancer screening can reduce your risk of illness or death from cancer.
- See your doctor if you notice blood in your poo, ongoing constipation or diarrhoea, or unexplained weight loss.
How your bowel works
Your bowel is made up of 2 main parts:
- the small intestine (small bowel), which absorbs nutrients from digested food
- the large intestine (large bowel), which absorbs water as digested food goes through it.
- Your bowel is part of your digestive system. Your digestive system turns everything you eat and drink into nutrients to fuel your body.
Your digestive system is a long, muscular tube that starts at your mouth and ends at your anus. It includes your:
- mouth
- oesophagus – a tube that connects the mouth and throat to the stomach
- stomach – an organ that breaks food down before it goes into the small intestine
- small intestine – a tube that connects the stomach to the large intestine
- large intestine – where poo is made before it leaves the body through the rectum and anus.
Depending on what you’ve eaten and other factors, it can take 23 to 37 hours for food to travel through your digestive system.
Your rectum (the last part of the large intestine) stores poo and signals you need to go to the toilet.
Your anus (the end of your large intestine) has anal sphincters that keep your large intestine closed until you’re ready to poo. They are supported by your pelvic floor muscles to help control your bowel movements.
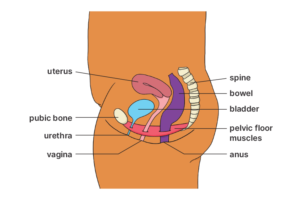
How your pelvic floor supports your bowel
Your pelvic floor is made up of muscles and tissues that stretch from your tailbone to pubic bone. It acts like a supportive hammock for your bowel, bladder and uterus. It’s important to keep your pelvic floor muscles strong.
How to have good bowel health
Good bowel health is more than being regular. Signs of a healthy bowel include:
- doing soft, formed poos
- being able to hold on for a short time when you feel the urge to poo
- pooing without straining or feeling pain
- completely emptying your bowel when you go to the toilet.
Learn more about bowel health on the Continence Health Australia website.
What’s normal?
It’s normal to poo from 3 times a day to 3 times a week.
Your poo should be soft, shaped like a sausage, and easy to pass. It should take you one to 2 minutes to empty your bowel. If it takes longer, you may be constipated or have a bowel-emptying problem.
The colour of your poo is almost always brown due to bile, a fluid produced by your liver to help digestion. Sometimes what you eat, for example, beetroot or liquorice, can affect the colour of your poo.
It’s also normal for your poo to smell.
What’s not normal?
Bowel habits vary from person to person, but there are some symptoms you should discuss with your doctor.
Look out for:
- blood in your poo, around the toilet bowl or on the toilet paper
- very dark or black poo
- very light-coloured poo
- much narrower poos than normal.
Also talk to your doctor if you notice:
- a sudden change in your bowel pattern
- unexplained weight loss
- accidental leakage of poo (bowel incontinence)
- an urgent need to poo without much time to get to the toilet (urge incontinence)
- hard, dry poo that’s difficult to pass (constipation), especially if it’s persistent
- loose, watery poo (diarrhoea), especially if it continues for more than 2 to 3 days
- frequent wind pain, cramps or bloating
- feeling that your bowel hasn’t been fully emptied after going to the toilet
- pain or a lump in your belly, anus or rectum.
There are many things you can do to have good bowel health.
Eat healthy food
It’s important to:
- eat a healthy diet, including foods that are high in fibre such as whole grains, fruits and vegetables
- have regular meals – try not to skip meals, as eating helps to move food through your digestive tract
- drink water regularly throughout the day.
Do physical activity
- Stay active to help move food through your digestive tract.
- It can also help to do pelvic floor exercises. Watch this Continence Health Australia website video about pelvic floor muscle exercises.
Have good toilet habits
Try to:
- do a poo when you get the urge
- relax when sitting on the toilet, and give yourself enough time so you don’t rush or strain.
- use the right sitting position on the toilet (sit with a straight back and lean forward with your elbows on your knees)
- avoid straining or holding your breath when doing a poo.
Be bowel aware
It’s important to be aware of your bowel pattern so you notice when something changes. See your doctor if you have any concerns – and ask them about bowel cancer screening.
Read the Looking After Your Bowel Guide on the Continence Health Australia website.
How your gut affects bowel health
Your gut includes your:
- stomach
- small intestine
- large intestine.
It has different types of bacteria (also known as the gut microbiome). Your genetics and diet influence your gut microbiome.
The more species of bacteria you have in your gut, the healthier it is. A healthy gut may have more than 1,000 species of bacteria.
Poor gut health is linked to many health problems, including:
- obesity
- diabetes
- heart disease
- anxiety
- skin conditions
- inflammation associated with autoimmune conditions (e.g. Crohn’s disease and coeliac disease).
How to improve your gut health
You can improve your gut health by eating high-fibre foods. Good sources of fibre include:
- fruit
- vegetables
- legumes (e.g. beans, chickpeas, lentils)
- wholegrains (e.g. oats, brown rice, corn).
It may also help to:
- eat a variety of unprocessed foods of many different colours
- eat food with live bacteria every day (e.g. pot-set yoghurts, kefir, kimchi, sauerkraut, kombucha, fermented pickles)
- reduce artificial sweeteners and food additives.
But we need more research to understand how these impact gut health.
Bowel cancer screening
Bowel (colorectal) cancer is when cancerous tissue grows inside the lining of the large intestine. It’s the fourth most common type of newly diagnosed cancer in Australia.
About half of people diagnosed are women. The risk increases with age, but if the cancer is found early, you have a very good chance of survival.
It’s important to have regular bowel cancer screening as it can detect blood in your poo before you notice it, reducing your risk of illness or death from cancer.
What is bowel incontinence?
Bowel incontinence is when you can’t control your bowel movements. It can range from an occasional leakage of poo to a complete loss of bowel control.
Many women have bowel incontinence at some time in their lives.
Causes of bowel incontinence
Bowel incontinence may be caused by weakened or damaged pelvic floor muscles and muscles around the anus.
Some possible causes are:
- pregnancy
- childbirth
- chronic constipation
- swollen veins around the anus or lower rectum (haemorrhoids)
- pelvic surgery
- pelvic radiation therapy
- certain medical illnesses (e.g. IBS)
- nerve damage from conditions such as diabetes
- the rectum coming out of the anus (prolapse).
How to get a diagnosis of bowel incontinence
If you’re worried about incontinence, talk to your doctor. They will ask about your medical history and symptoms. They may also ask you to keep a diary of your bowel habits and list what you eat and drink for 7 days.
During your appointment, your doctor may do a physical examination. This might include checking your:
- belly
- anus and anal sphincters
- pelvic floor muscles
- rectum.
You can ask your doctor to explain what they will do and tell them if you don’t feel comfortable with any parts of the examination.
You might need to do some tests. For example:
- a test to check your anal reflexes and sensations
- an ultrasound to check the rectum and the anal sphincters.
Prevention and management of bowel incontinence
You may be able to prevent and manage bowel incontinence with diet and lifestyle. For example:
- drink plenty of fluid (preferably water) each day
- reduce caffeinated and alcoholic drinks
- eat a healthy diet with a variety of foods that contain fibre
- stay active
- do regular pelvic floor muscle exercises
- learn how to use your pelvic floor muscles to hold on until you get to the toilet and relax when you sit on toilet.
Medicine or surgery may be used to treat some types of bowel incontinence.
You can:
- get help from a continence health professional, such as a pelvic floor physiotherapist or nurse continence specialist
- contact the National Continence Helpline.
Learn more about good bowel health.
Understanding irritable bowel syndrome (IBS)
Irritable bowel syndrome (IBS) is a chronic gut disorder that affects your stomach and intestines.
IBS is a group of symptoms, such as pain and bloating in your belly (abdomen) and changes in your bowel movements, for example, constipation and diarrhoea.
About 4% of the population have IBS. It’s more common in women, especially those aged 18 to 39 years.
Symptoms of IBS
Symptoms of IBS may include:
- recurrent belly pain, cramping or bloating that often eases after doing a poo or farting (passing wind)
- alternating constipation and diarrhoea
- changes in how your poo looks
- changes in how often you do a poo
- farting.
These bowel symptoms may not be related to IBS. It’s important to see your doctor if you’re concerned about any changes to your bowel habits.
Causes of IBS
Commonly accepted causes of IBS include:
- diet (food intolerances)
- stress
- gut infections (gastroenteritis)
- medicines
- problems with signals between the brain and gut.
How to get a diagnosis of IBS
There are no tests to diagnose IBS. Your doctor will usually diagnose IBS based on your symptoms and how often you experience them.
Treatment and management of IBS
Your doctor will recommend lifestyle changes to decrease IBS symptoms.
You may need to increase the amount of fibre in your diet and follow a low FODMAP diet. FODMAPs are a group of sugars that your body doesn’t absorb properly. It’s a good idea to get advice from a dietitian so you don’t miss out on any important nutrients.
Lifestyle changes include reducing stress with relaxation techniques and increasing physical activity.
While everyone is different, you can try to:
- avoid food that aggravates your symptoms – these could include dairy, onion, cabbage, Brussels sprouts, dried beans and lentils
- drink plenty of water each day
- avoid drinks that aggravate your symptoms (e.g. caffeinated drinks, fizzy drinks and alcohol)
- reduce artificial sweeteners.
To relieve constipation, try:
- prunes
- pear juice
- soluble fibres (e.g. psyllium)
- over-the-counter products to help soften your poo.
If you have persistent diarrhoea, try medicines such as loperamide.
Psychological therapies, such as cognitive behaviour therapy (CBT) and hypnotherapy may also help reduce IBS symptoms.
Our review process
This information has been reviewed by clinical experts and is based on the latest evidence.
Our content review process ensures our health information is accurate, trustworthy, current and useful.
We regularly check our information to make sure it reflects the latest clinical guidelines and key findings from large, reliable studies.
Where possible, we focus on Australian research to make our information more relevant locally.
Experts play a key role in reviewing our content. Clinicians at Jean Hailes check information for accuracy and real‑world relevance. These include GPs, gynaecologists, endocrinologists, psychologists and allied health professionals.
We also work with partner organisations, independent specialists and people with lived experience to make sure our content reflects both expert knowledge and the experiences of the community.

Want to learn more about your bowel?
Ever wondered if you have good bowel health? In this Q&A, Bowel Cancer Australia’s Dr Penelope De Lacavalerie explains why checking your poo regularly is something we all should do.













