In this Medical Observer article for health professionals, Jean Hailes endocrinologist Dr Sonia Davison and specialist surgeon Mr Su-Wen Loh discuss the high-risk and challenging elements of dense breasts.

Breast density is a strong predictor of breast cancer risk. Why is this so?
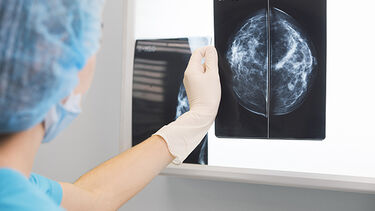
Breast density consists of the glandular elements and ductal structures of the breast. As breast cancer typically arises from ducts and glands, it makes sense that the risk of developing cancer in a dense breast is higher than in a non-dense breast. What makes this tricky is the fact that breast density reflects white on a mammogram. Sinister pathology can also reflect as white.
Overlapping breast tissue, with or without pathology, superimposes very white, or opaque, on a mammogram. This makes it difficult to see the abnormality within the normal white cloud, lowering diagnostic yield. So reading the patient's mammogram is a great challenge.
A review by Curtin University and the University of Western Australia, recently published in the journal Climacteric, reinforces the need for breast density to be incorporated in the screening process. There is a growing consensus that including breast density in a mammogram report will give clinicians further valuable information in terms of assessing an individual's breast cancer risk.
The Royal Australian and New Zealand College of Radiologists recommends density be mentioned on mammogram reports. The federal government has agreed to review the growing evidence about the importance of breast density, with a view to updating BreastScreen Australia's position. It is likely to make a decision by the middle of this year. Many radiologists already preface their reports with a comment on breast density. This gives us an indication of their thoughts on the patient's background risk, and also how confident they are about reading the patient's mammogram.
Several things can be done to manage the risk associated with breast density. To help overcome 2D (superimposed) density on a mammogram, newer 3D mammograms, or tomograms, provide better diagnostic yield by taking multiple shots from different angles. This gives rise to a mini CT scan of the breast. Many screening centres routinely use a 3D mammogram. Many diagnostic outlets also perform 3D mammography as a standard. It's fair to assume that in the near future 2D mammograms will be completely replaced by 3D tomograms.
Ultrasound is a good adjunct. Careful examination of dense tissue with sonography helps exclude solid lesions not easily seen on the superimposed mammogram. Adding a breast ultrasound to complement your patient's dense mammogram will certainly give the investigator more confidence in reporting. A breast MRI is a 3D study of the breast with contrast infusion (IV Gadolinium). Volumetric analysis with contrast (3D computer rendering) details breast tissue clearly and bypasses the problem of overlapping density. There are, however, contraindications to an MRI, and contrast MR requires normal kidney function.
There is not yet a gold standard method of determining breast density. Although there are multiple methods used to determine breast density, it is still unclear which method provides the strongest predictor of breast cancer risk. Estimation of breast density is quite subjective, and very much dependent on the reporting radiologist or clinician. At present, the most common measurement of breast density is the Breast Imaging Reporting and Database System (BIRADS).
More research needs to be done to determine screening recommendations for women with dense breasts. There are currently randomised controlled trials (eg, DENSE trial and WISDOM study) taking place in other countries. However, the results may not be translatable to the Australian setting. Further research, particularly local, is needed to understand the primary prevention options for women with dense breasts.
Jean Hailes is proud to provide a monthly column in the medical newspaper, Medical Observer. Designed to give GPs and health professionals a short informative summary of important women's health topics and conditions, these articles provide practical information to inform and enhance clinical practice.
Dr Sonia Davison is an endocrinologist in private practice at Jean Hailes, with interests in gynaecological and general endocrinology. She is also a Senior Postdoctoral Research Fellow in the Women's Health Research Program, Monash University.
Mr Su-Wen Loh is a breast surgeon in both public and private practice. He works closely with Jean Hailes' doctors and patients. After completing his general surgical training in Melbourne, Su-Wen completed a breast cancer fellowship in Cambridge, UK.
All reasonable steps have been taken to ensure the information created by Jean Hailes Foundation, and published on this website is accurate as at the time of its creation.
© 2024 Jean Hailes Foundation. All rights reserved. This publication may not be reproduced in whole or in part by any means without written permission of the copyright owner. Contact: licensing@jeanhailes.org.au