Fibroids are noncancerous growths found in the muscle wall of the uterus. Many women have fibroids. There are different treatments, depending on the type, size, number and location of your fibroids. Learn more about the symptoms, causes, diagnosis and treatment options.
What are fibroids?
Symptoms
Causes
Diagnosis
Fertility and pregnancy
Treatment and management
When to see your doctor
Related resources
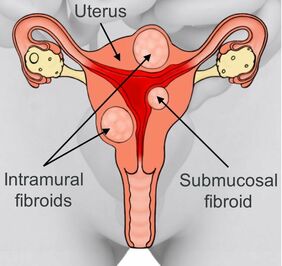
Fibroids are noncancerous growths found in the muscle wall of the uterus. They can grow on the outer wall of the muscle (subserosal), within the muscle wall (intramural), on the inner wall lining the cavity of the uterus (submucosal), or a combination of these.
Fibroids can vary in size from a pea to a rockmelon or bigger.
This condition occurs in up to 70% of women aged under 50. After menopause, fibroids usually shrink and may disappear.
The below picture shows a uterus with different types of fibroids.
About 20% to 30% of women experience some symptoms related to fibroids.
For example:
Other symptoms include:
We don’t know exactly what causes fibroids, but we do know the female hormones oestrogen and progesterone stimulate the growth of fibroids.
Some factors may increase the risk of fibroids.
For example:
Fibroids can be diagnosed in different ways.
For example:
Talk to your doctor or specialist about the potential benefits and risks of each option before you decide.
Fibroids can affect fertility, depending on their size and location. Fibroids may also cause miscarriage or early labour. In some cases, caesarean section may be recommended for future births.
Most fibroids don’t require treatment unless you are planning to get pregnant, or symptoms such as period pain and heavy bleeding stop you from doing things you normally do.
If fibroids don’t affect your daily life, you can choose to leave them untreated and simply increase iron and vitamin C in your diet.
Treatment will depend on your symptoms and the size, number and location of your fibroids.
Your doctor may recommend different medical treatments, such as mefenamic acid, tranexamic acid or hormonal treatments (e.g. the combined oral contraceptive pill or Mirena® IUD).
Your doctor may recommend a combination of medicines and hormones to shrink your fibroids, usually if infertility is an issue. After you stop treatment, your fibroids can grow back.
You may be able to treat your fibroids with radiological treatment.
For example:
You may need different types of surgery to remove fibroids. The surgery will depend on the size and position of your fibroids.
For example:
Talk to your doctor or specialist about the potential benefits and risks of each option before you decide.
See your doctor straight away if you experience symptoms such as:
This web page is designed to be informative and educational. It is not intended to provide specific medical advice or replace advice from your health practitioner. The information above is based on current medical knowledge, evidence and practice as at April 2023.
This content has been reviewed by a group of medical subject matter experts, in accordance with Jean Hailes policy.
© Jean Hailes Foundation. All rights reserved. This publication may not be reproduced in whole or in part by any means without written permission of the copyright owner. Contact: licensing@jeanhailes.org.au